Team approach to lupus care being tested at Duke Health
Effort is aimed at addressing barriers faced by patients, provide equitable healthcare
A new project incubating at Duke Advanced Practice Provider Leadership Institute (APPLI) seeks to foster a team approach to lupus care at Duke Health in Durham, North Carolina.
The project is being led by Keisha-Gaye O’Garo, a clinical psychologist, and Karen McCain, a psychiatric nurse practitioner, both from Duke University School of Medicine.
Both recognized the need to address barriers faced by lupus patients and provide equitable healthcare. Lupus is a complex, long-term disease that requires input from various medical specialists, making a team approach essential. It causes skin rashes, joint pain, and fatigue. Its symptoms can be mild to severe and can come and go. There is no cure, but symptoms can improve if treated early.
Anyone can develop lupus, but it occurs more often in women. It’s also more common in those with a family history of the disease and in Black and Latino communities.
“We decided to target lupus because it has extremely high mortality rates for Black females, in some cases at a very young age,” O’Garo said in a university news release. “And we need to start talking to one another about how to address some of the barriers they face and ensure we’re providing equitable health care.”
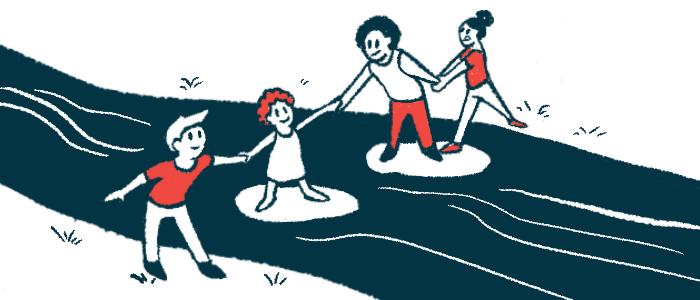
The project features a rheumatologist, physician assistant, nurse practitioner, clinical social worker, psychologist, registered dietitian, and physical therapist working as a team to provide comprehensive care. The approach draws inspiration from a care model O’Garo saw during an internship at an intensive pain program for veterans.
“I saw this amazing change in veterans who came in disappointed, discouraged, even disillusioned, and by the time they left the program, they were using nonpharmacological interventions,” O’Garo said. “I’d see hope in their eyes, and excitement, and a sense of control and confidence.”
Developing a new approach to lupus care
APPLI, supported by the Duke Health Chancellor’s Office, is a yearlong program that provides coaching, skills training, and project development support to developing health equity leaders.
“It’s a professional development fellowship where our participants strengthen their individual and team-based leadership and management skills,” said Anh Tran, PhD, who’s directed APPLI since its launch 10 years ago. “It’s also structured like a project incubator model — the teams come in with a vision, and we provide them with coaching, new skills, and project development and management infrastructure to help them make that vision become a reality.”
The Duke Young Adult Rheumatology Clinic, directed by rheumatologist Rebecca Sadun, MD, PhD, served as the setting to implement the project. Sadun’s team included Lisa Ray, a physician assistant, and Anne Fields, a clinical social worker.
McCain, with Sadun, Ray, and Fields, meets patients and identifies those who may benefit from counseling or medication, or both. McCain also optimizes medication to get the best results from it.
O’Garo provides patients strategies for coping with pain, reducing stress, getting better sleep, and setting boundaries to manage their disease.
“For many patients, anger starts to well up because they feel disappointed and betrayed by their bodies,” O’Garo said. “I try to help them really listen to, engage with their body, and make decisions based on what their body is saying, so they can achieve that peace, that sense of life satisfaction, that control they’re looking for.”
Sadun’s team has grown to include Sally Dunn, a physical therapist, and Maria Tucker, a registered dietitian. Dunn, a Pilates specialist, helps patients set up a plan to stay active without pushing themselves too hard.
“Quite a few of our patients have been on chronic high-dose steroids, which has resulted in weight gain, and they have a lot of pain, so it’s challenging for them to be physically active,” Sadun said.
So far, the approach has been positive and patients have seen improvements in life satisfaction, cognition, body image, sleep, physical health, and social support.
The team members are also learning from each other and this has helped reduced burnout and secondary traumatic stress. They’re motivated to expand the project and are adding a coordinator, case manager, and an acupuncturist to the team, as well as offering educational programs and support groups.
“I’m grateful to the APPLI program for giving me this opportunity,” O’Garo said.