Specific T Cell Subset Contributes to Disease Progression in New-Onset Patients with SLE
Written by |
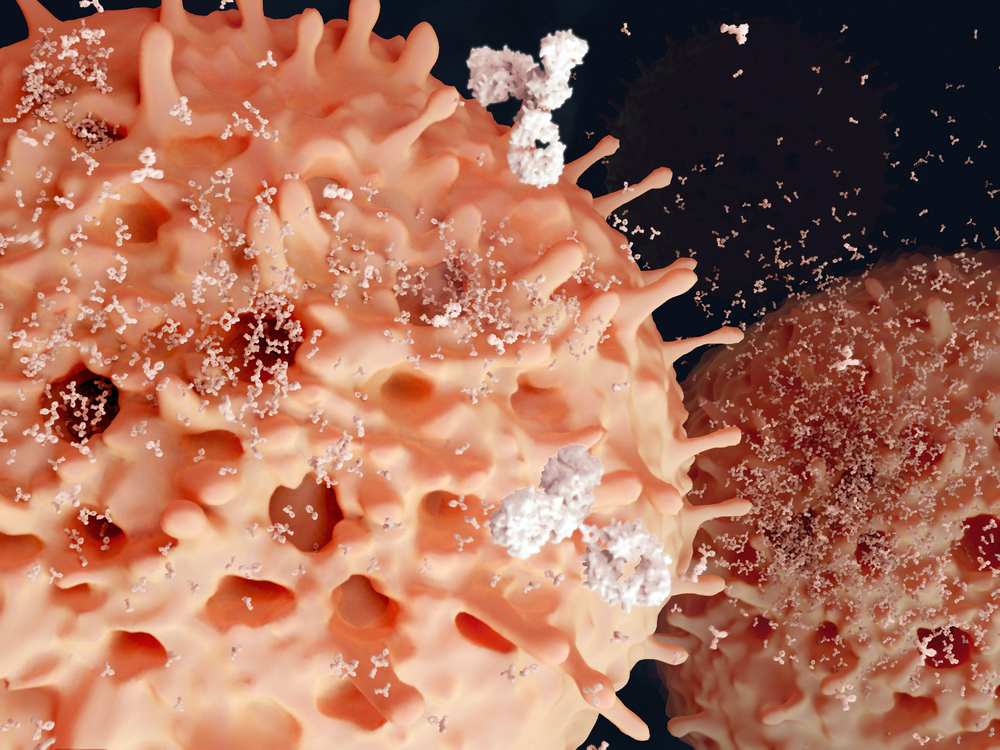
In a recent study entitled “Hyperactivation and in situ recruitment of inflammatory Vδ2 T cells contributes to disease pathogenesis in systemic lupus erythematosus” scientists discovered that the biggest human γδ T cell subset, the Vδ2 T cells present in peripheral blood, are key mediators of tissue injury and disease progression in newly-onset patients with systemic lupus erythematosus. The study was published in the journal Scientific Reports.
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by a wrongful action of the immune system against healthy tissue which induces autoantibody production against oneself. The disease affects skin, joints, kidneys, brain, among other organs and is much more common in women than men. Additionally, tissue injury in SLE is caused by local recruitment of inflammatory cells.
In this study, researchers investigated whether a subtype of key immune regulators, the T cells, contributes to autoantibody production and is directly recruited to local tissues to participate in tissue injury. The specific subset under study is called Vδ2, the major human γδ T cell subset in peripheral blood (i.e., the blood that circulates through the heart, arteries, capillaries, and veins and is the main means of transport within the body).
The team discovered that in peripheral blood the number of circulating Vδ2 T cells is significant lower in new-onset SLE patients when compared to healthy controls. Moreover, the team observed that reduction in Vδ2 T cell number correlated with SLE severity, as measured by the SLE Disease Activity Index (SLEDAI) score. Specifically, patients developed worse proteinuria (the presence of abnormal quantities of protein in the urine), a clear sign of kidney damage and denoted by an increased penetration of Vδ2 T cells in the kidneys of patients with lupus nephritis (inflammation of the kidney caused by SLE). Researchers also observed that Vδ2 T cells of new-onset SLE patients had increased expression levels of several chemokine-receptors, including CCR4, CCR7, CCR8, CXCR1 and CX3CR1 therefore exacerbating the recruitment of inflammatory cells to tissues.
In light of these results, the team highlights that the levels of Vδ2 T cells in peripheral blood decreases significantly in new-onset active SLE patients as a result of their increased penetration in local tissues, and not due to increased cell death or decreased proliferation. Additionally, Vδ2 T cells act as inflammatory cells and contribute to disease progression by promoting tissue injury.




