Nitrated Nucleosome Levels Rise at Onset of Neuropsychiatric Event, Lupus Study Shows
Written by |
The levels of nitrated nucleosome (NN) in the blood rise at the time of a neuropsychiatric event in some patients with systemic lupus erythematosus (SLE), research from a multi-center, international study shows.
However, new studies are required to assess the potential of NN as a biomarker for neuropsychiatric systemic lupus erythematosus (NPSLE).
The study, “Nitrated nucleosome levels and neuropsychiatric events in systemic lupus erythematosus; a multi-center retrospective case-control study,” was published in the journal Arthritis Research & Therapy.
Currently clinicians have no easy test to assess if neuropsychiatric manifestations in SLE patients are due to active disease or to other, non-SLE causes.
Previous studies suggested autoantibodies or signaling molecules as potential biomarkers for NPSLE but “despite a large number of studies over the last 30 years none of these biomarkers has shown a robust association with either NPSLE in general or with any specific NPSLE manifestation,” researchers wrote.
Following previous evidence that nitration and nucleosome levels are associated with active SLE, researchers at University College London hypothesized that measuring the levels of nitrated nucleosomes could be a marker for NPSLE.
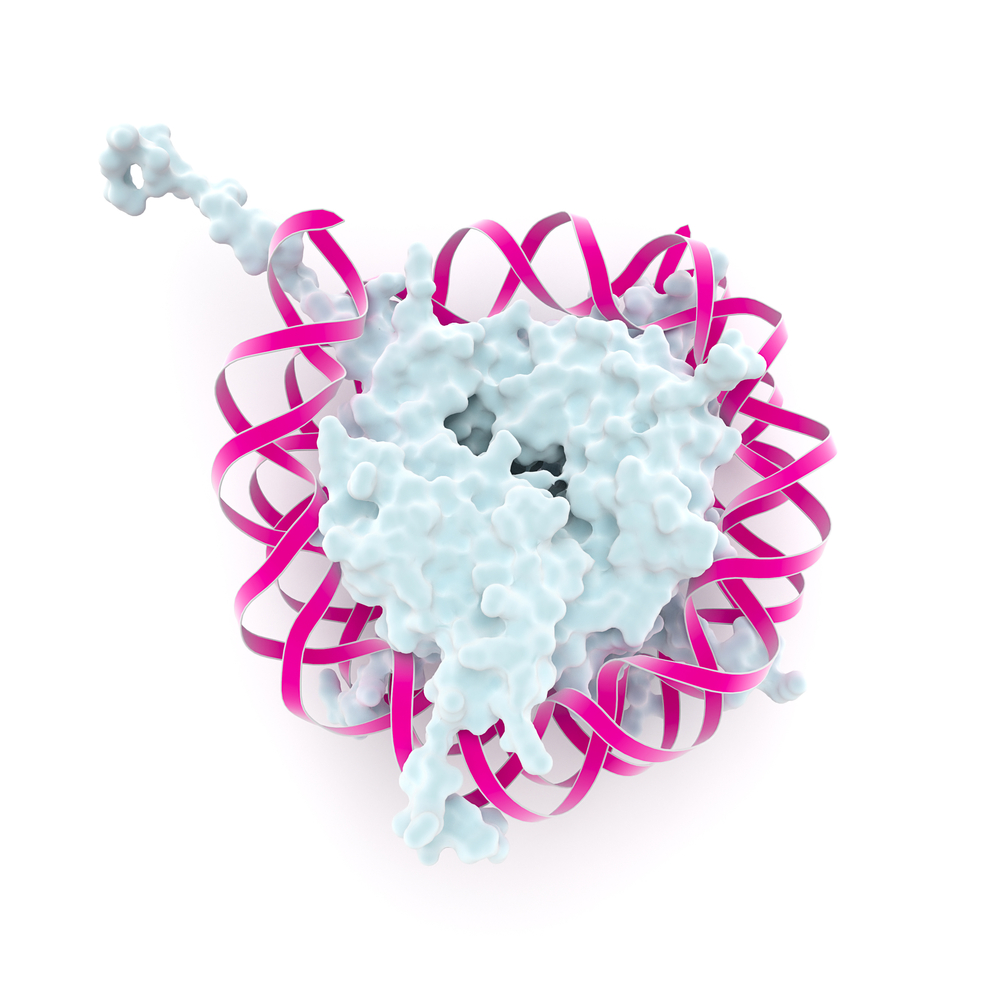
Nucleosomes – a mix of DNA and proteins – are released into circulation as cells die and are found in high levels in SLE patients. These patients also carry high levels of nitric oxide (the result of blood vessel inflammation), promoting nitration.
Researchers analyzed blood samples from 216 SLE patients with confirmed neuropsychiatric events, collected before, during, and after the NP event. As control participants, they looked at patients with SLE, but no recorded neuropsychiatric events. Each patient had two matched controls.
All samples were obtained from the large SLICC inception group – composed of 1,600 patients, recruited within 15 months of SLE diagnosis. Patients were recruited in 31 centers across North America, Europe, and Asia.
To determine whether a neuropsychiatric event was attributable to SLE, researchers followed the same predetermined classification rules used in previous studies – NP events that fulfilled criteria for model A or for model B were attributed to SLE.
“Those events that did not fulfill these criteria were attributed to non-SLE causes (non-A, non-B events),” they explained.
In total, they analyzed 26 patients with model-A NP events and 190 with non-A, non-B events.
They went on an explained that they included patients with NP events not attributed to SLE as a “a control group in which we did not expect to see a rising and falling pattern of serum NN.”
However, it was in this particular group of patients that researchers saw rising NN levels in the blood, compared to pre- and post-event NN levels, or to matched controls.
“We did not detect any similar statistically significant result in patients with model-A NP events, perhaps due to the much smaller numbers in that group,” they wrote.
Overall, “in this multi-centre study we found that serum NN levels rise at the time of an NP event in a proportion of patients with SLE, including some cases of headache,” the study concluded.
Future studies are required to assess if measuring the levels of NN in the blood is a potential biomarker for NPSLE.




