Dendritic Cells May Hold Key for New Lupus Immunotherapy, Study Reports
Written by |
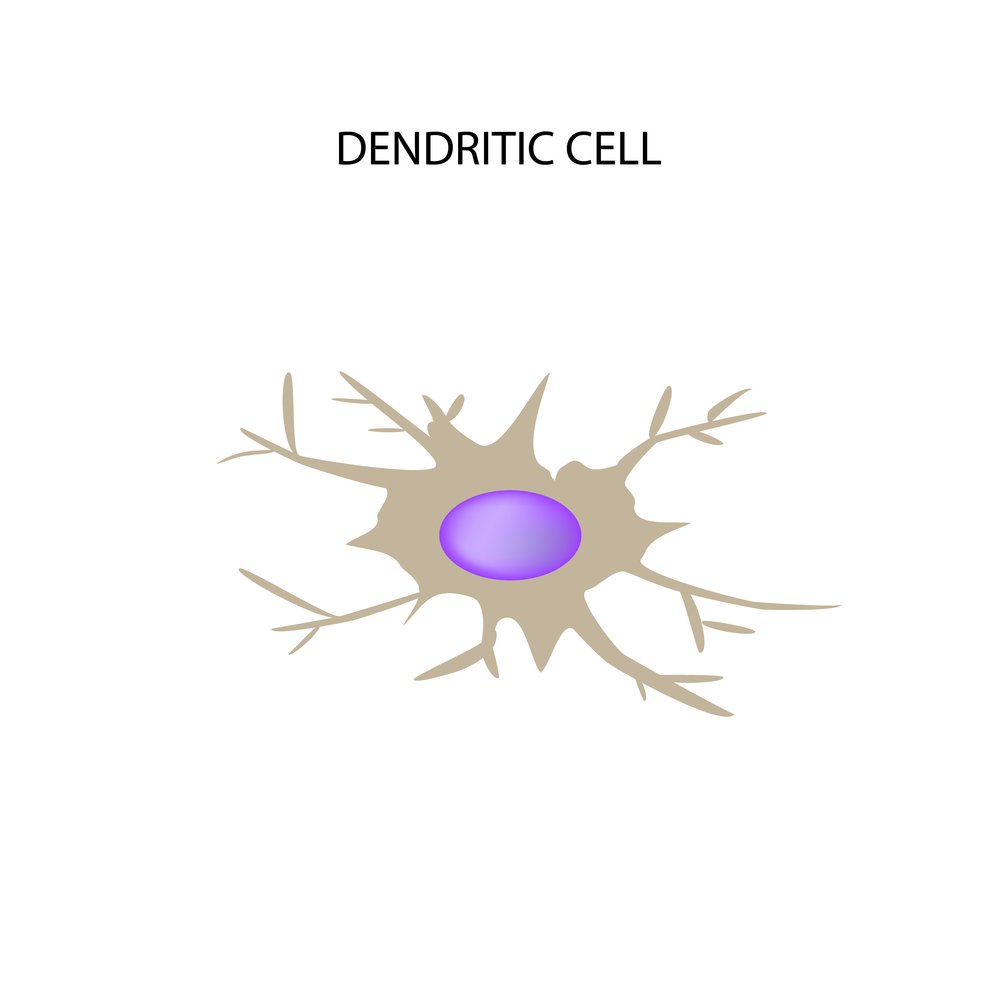
Re-engineering a class of immune cells called dendritic cells (DCs) toward self-tolerance for many of the antigens underlying systemic lupus erythematosus (SLE) may be a potential therapeutic approach to treat lupus patients and other autoimmune diseases, according to a recent study.
Findings from the study, “Autologous tolerogenic dendritic cells derived from monocytes of systemic lupus erythematosus patients and healthy donors show a stable and immunosuppressive phenotype,” were published in the journal Immunology.
SLE is an autoimmune disease characterized by the presence of auto-antibodies against nuclear components. One of the processes responsible for generating autoantibodies is the death of cells, called apoptosis. In SLE, apoptosis is increased and is considered to contribute to the development of the disease. Therefore, “it is reasonable to hypothesize that loss of tolerance towards dead cell-related epitopes is intimately linked to SLE onset,” researchers wrote.
Dendritic cells are a group of immune cells known for their ability to regulate adaptive immune responses, but also self-tolerance (when the immune system does not attack the body’s own proteins).
In this study, researchers hypothesized that since DCs can be generated in vitro (in a lab culture dish) to exhibit tolerance for specific antigens — the proteins that induce an immune response — they could be delivered to SLE patients to correct their dysfunctional immune responses.
Previous studies have used two compounds — rosiglitazone (RGZ) and dexamethasone (DEXA) — to prevent generation of antinuclear antibodies and help generate human tolerogenic DCs (tolDCs).
Now, researchers have extracted dendritic cells from healthy people, called controls, and SLE patients. The cells were then treated with both immunomodulatory drugs, DEXA and RGZ, to induce tolDCs. They used the subject’s own immune cells and induced cell death by ultraviolet irradiation.
The apoptotic cells were then given to tolDCs as a source of self-antigens so that the tolDCs could restore tolerance to specific auto-antigens. They then tested the functionality of tolDCs, to see if they were capable of suppressing the activation of T-cells.
In ex vivo experiments (in mammals), the authors observed that indeed, tolDCs suppressed the activation, proliferation, and cytokine secretion of CD4+ T-cells. Most importantly, this suppression was also observed using T-cells from an SLE patient.
Overall, this study reports the first-time generation of tolDCs directed to relevant self-antigens involved in lupus disease. This represents a strategy for restoring immune tolerance, which may be a potential therapeutic approach for treating this and other types of autoimmune diseases.