Immune Response Regulator Interferon-Gamma Is Associated with Cerebral Atrophy in Lupus, Study Suggests
Written by |
Interferon-gamma, an endogenous regulator of immune responses, is associated with reduced cerebral volume in lupus patients, a new Brazilian study shows.
The study, “Interferon-γ Is Associated with Cerebral Atrophy in Systemic Lupus Erythematosus,” appeared in the journal Neuroimmunomodulation.
The research was led by Simone Appenzeller, MD, PhD, from the Rheumatology Unit and the Neuroimaging Laboratory at the Biology Institute at State University of Campinas in Brazil.
Nearly 75% of lupus patients have involvement of the central nervous system (CNS), but problems such as the lack of a single diagnostic test and poorly understood molecular mechanisms have largely hampered proper management of these patients.
Patients with neuropsychiatric lupus have increased levels of autoantibodies, which attack a patient’s own tissues, and cytokines (molecules produced and released by cells of the immune system) when compared with other lupus patients and healthy individuals. Researchers believe that cytokines in the cerebrospinal fluid (CSF), the fluid that surrounds the brain and spinal cord, may be toxic and may promote vascular damage.
Furthermore, the presence of a large number of lymphocytes and higher concentrations of proteins may also be observed in some lupus patients with CNS involvement.
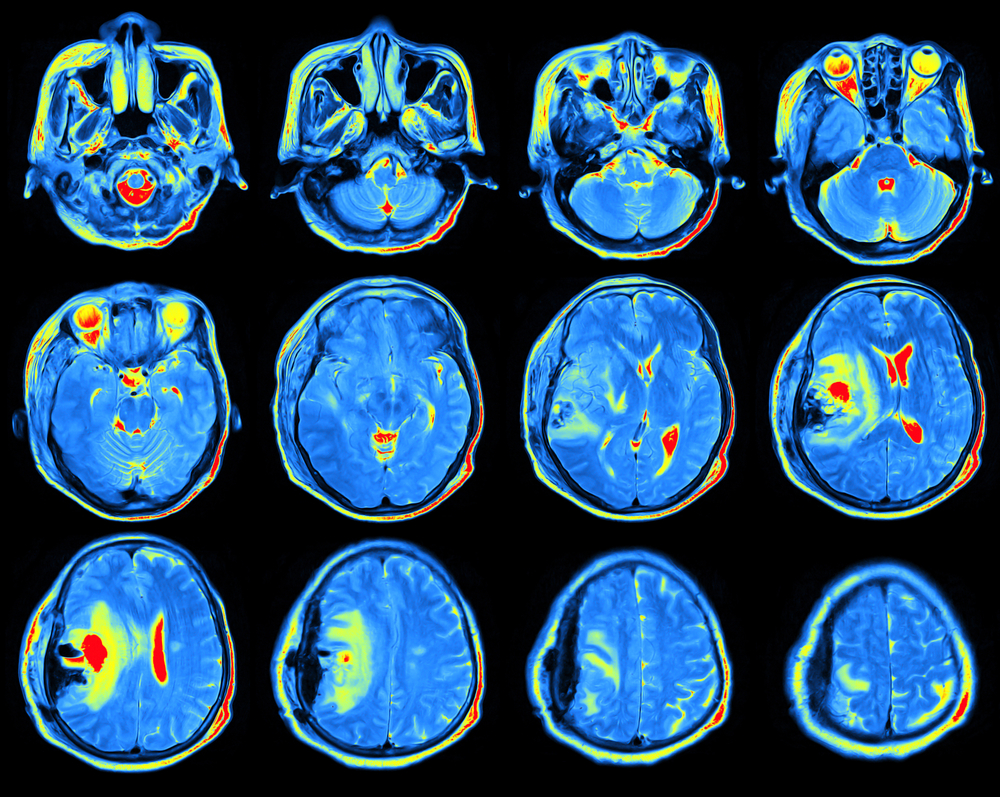
Therefore, the team set out to study the CSF cytokine profile and magnetic resonance imaging (MRI) in lupus patients with CNS involvement.
The final cohort included 20 adult lupus patients, of whom 18 were women, with active CNS manifestations. These patients were compared with healthy controls matched for age and sex.
The researchers conducted MRI scans and collected blood and CSF from the patients to determine the levels of several proteins, antibodies, and cytokines. The authors observed that measuring multiple cytokines may help predict treatment outcome in neuropsychiatric lupus patients.
The results showed higher levels of several cytokines in the CSF of lupus patients, including IL-12 p40/p70, IFN-gamma, TNF-alpha, and IL-10. High lymphocyte levels in CSF was observed in eight (66%) patients, which the scientists attributed to higher IFN-gamma levels.
Furthermore, three patients (15%) showed demyelinating lesions — a disruption of the myelin sheath, a protective cover of nerve fibers — and five patients (25%) had cerebral atrophy, which may be caused by disease activity and corticosteroid treatment. Also, 12 patients (60%) showed ischemic lesions, which generally result from insufficient blood supply.
The scientists observed that cerebral lesions were associated with CNS manifestations and cumulative damage, and that lupus patients showed reduced cerebral volume when compared to controls. A correlation also was found between cerebral volume reduction and IFN-gamma levels in the CSF.
Overall, the results show that although lupus patients with CNS manifestations had increased levels of several cytokines in the CSF, “only IFN-gamma was associated with a cerebral volume reduction in SLE, suggesting an immunological basis for global atrophy in SLE,” the authors wrote.
“Recognition of potential biomarkers through CSF cytokine profiling … could have diagnostic utility and might provide new insights into the disease pathogenesis,” they added.





