Mitochondria Protein Triggers Immune Response in Lupus Patients, Study Reports
Reactive oxygen species in cells’ mitochondria trigger an immune response widely detected in patients with lupus, researchers have discovered.
The finding suggests the potential for a new therapeutic avenue to ameliorate the effects of the chronic autoimmune disease.
The study, “Reactive oxygen species induce virus-independent MAVS oligomerization in systemic lupus erythematosus,” was published in the journal Science Signaling.
Patients with systemic lupus erythematosus (SLE) exhibit excessive production of type I interferon (IFN), a response triggered during viral infections. The mechanism that triggers the type I IFN response in lupus has remained unknown, however.
Scientists at the University of Vermont’s Larner College of Medicine discovered that a mitochondria protein, called mitochondrial antiviral-signaling protein (MAVS), can trigger type I IFN production in SLE patients with no signs of viral infection.
“Typically, this protein — mitochondrial antiviral signaling or MAVS — is responsible for recognizing viral infections,” Dr. Iwona A. Buskiewicz, the study’s first author, said in a press release. Her team’s study is “the first paper showing that the interferon pathway can be activated by something other than viral infection or nucleic acids,” she said.
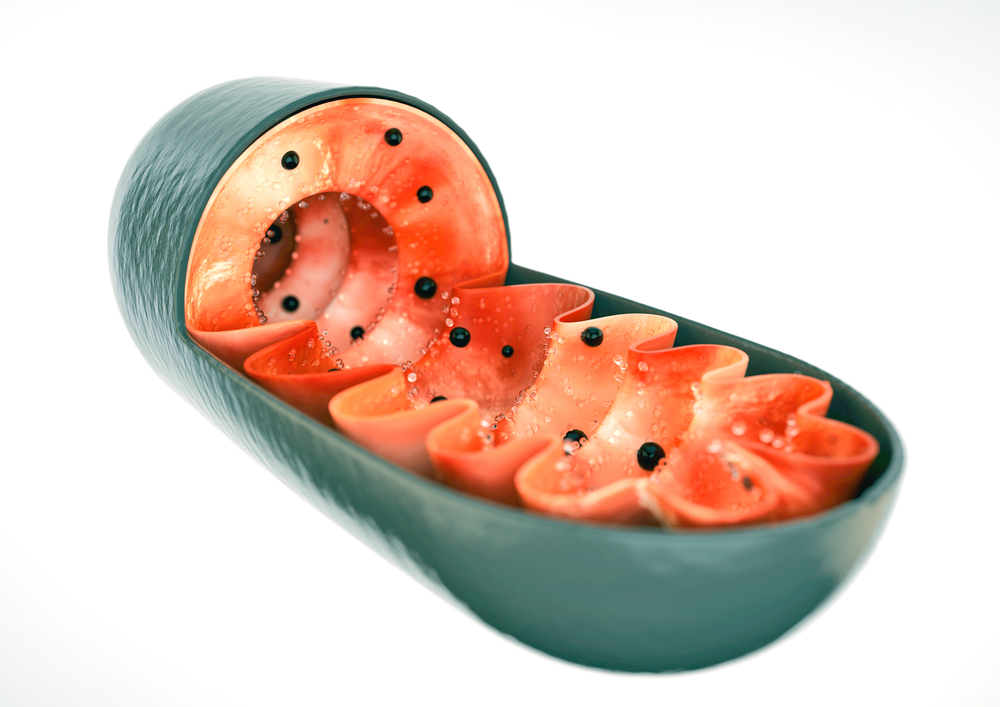
Mitochondria are small organelles within our cells commonly known as the cells’ powerhouses, or energy producers.
Scientists have discovered that reactive oxygen species (ROS) produced by mitochondria trigger the clustering of MAVS driving IFN production. When ROS were inhibited, scientists were able to prevent MAVS oligomerization — or the joining together of several MAVS molecules — and, consequently, to avoid type I IFN production.
The results suggest that mitochondria oxidative stress, or ROS buildup inside cells, promotes a type I IFN response in lupus patients. The findings also suggest that targeting MAVS is a potential therapeutic strategy directed towards mitochondria that could prove beneficial for SLE patients.
“We need to develop a drug that can revive the mitochondria,” Buskiewicz said. “A more focused antioxidant therapy targeting the particular organelle may have more efficacy.”
The researchers are now collaborating with rheumatologists to explore this potential therapy. A starting point will be analyzing how levels of MAVS oligomerization and type I IFN response change in antioxidant therapy.





