Rituxan Could Be Alternative Therapy in Patients with Neurological Issues, Case Report Indicates
Written by |
Rituxan (rituximab) could be a valid alternative to standard of care in systemic lupus erythematosus (SLE) patients with neurological and psychiatric manifestations, a new Italian case report shows.
The research, “Severe neuropsychiatric systemic lupus erythematosus successfully treated with rituximab: an alternative to standard of care,” was published in the journal Open Access Rheumatology: Research and Reviews.
The study’s corresponding author is Matteo Piga, MD, from the Rheumatology Unit, University Clinic AOU of Cagliari, in Cagliari, Italy.
Neuropsychiatric involvement in lupus (NPSLE) leads to higher risk of hospitalization and reduced quality of life. In particular, demyelination (damage to the myelin sheath that covers neurons and is critical for proper neuronal communication) caused by lupus is a rare, life-threatening condition with high risk of disability and death.
Recommendations from the European League Against Rheumatism (EULAR) include a two-step approach in severe inflammatory NPSLE, with cyclophosphamide and intravenous corticosteroids to control inflammation and prevent irreversible damage, followed by immunosuppressive maintenance therapy to prevent relapse and spare the use of steroids, which can induce new NPSLE events.
Depletion of B-cells (a type of immune cells) with Rituxan is a successful second-line treatment in patients with refractory and relapsing NPSLE, by inhibiting immune response and decreasing production of pro-inflammatory molecules. Rituxan, developed by Genentech and Biogen, has been considered as first-line treatment in lupus to decrease the steroid burden, but remains limited to patients who show inadequate response to conventional immunosuppression.
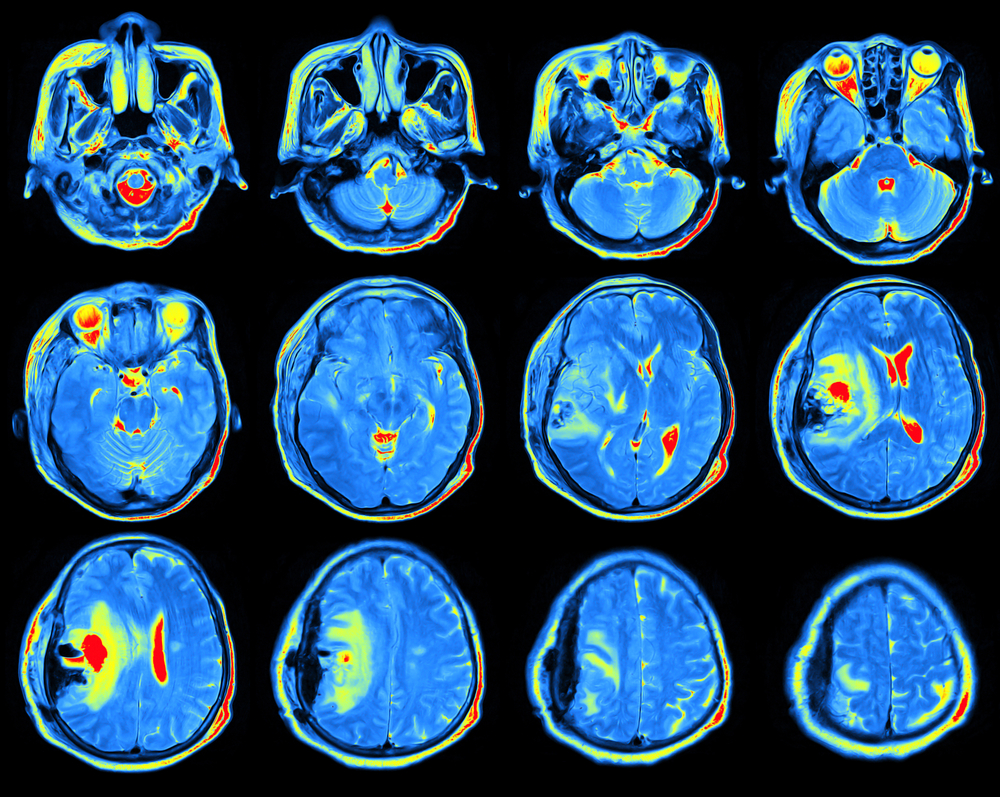
The authors discuss the potential use of Rituxan as a two-step strategy in severe inflammatory NPSLE. They report on a 49-year-old woman with lupus and severe and progressive cognitive impairment, cranial nerve palsies, weakness and sensory loss in limbs, worsening of renal function, and steroids-induced Cushing’s syndrome. Furthermore, damage in several areas of the brain and multiple mononeuritis (inflammatory damage in nerves) were observed.
The patient was diagnosed with active lupus and severe neurological impairment due to demyelination. Prescribed treatment included 500 mg methylprednisolone (PRE) pulses for three days, followed by one pulse of 500 mg cyclophosphamide, and 1 g Rituxan, which was repeated 14 days later. Maintenance therapy included PRE 25 mg per day, rapidly decreased to 7.5 mg/day in six months, and mycophenolate mofetil 1 g/day.
The clinicians observed progressive improvement in neurological dysfunction, with near complete resolution of brain lesions after one year. They conclude that the therapeutic strategy “was successful to lower inflammation, prevent accrue of damage, avoid new relapse and reduce the use of corticosteroids.”
Overall, Rituxan “could be considered as a possible alternative to standard of care in the management of severe inflammatory neuropsychiatric SLE, but it should be associated with a conventional immunosuppressant as maintenance treatment to reduce the risk of flare and reduce corticosteroids dose,” the team wrote.





