Lupus Researchers Identify Key to Autoreactive B-Cells, with Potential for Better Treatment Approach
Written by |
A study published in the Journal of Experimental Medicine demonstrates that a particular cell-signalling protein is crucial for the formation of autoreactive B-cells in systemic lupus erythematosus (SLE), but not for the formation of B-cells fighting infections.
The finding of this autoimmune mechanism opens up the possibility for the development of new, more specific therapies for lupus and other autoimmune diseases.
The hallmark of lupus, as well as other autoimmune diseases, is the activation of immune processes, normally targeted at invading pathogens and flawed cells that instead attack healthy tissues. The processes are mediated through the spontaneous production of autoreactive B-cells, producing tissue-destroying auto-antibodies.
B-cells are a variety of cells with different properties, and scientists still know little about about why and how different kinds of B-cells arise, including autoreactive ones.
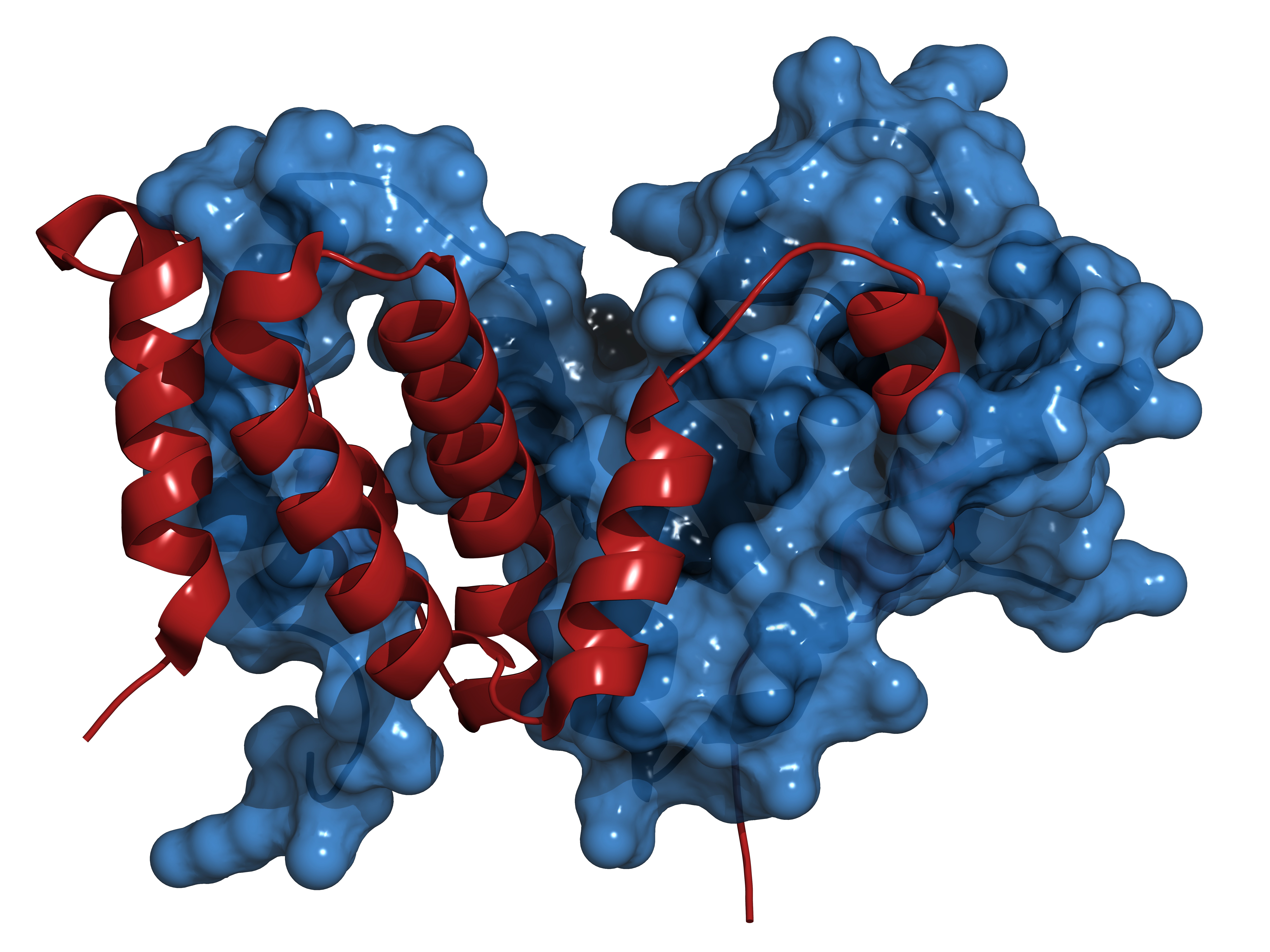
The immune signalling factor interferon-gamma has long been suspected to play a role in lupus, as patients have increased levels of this factor and mouse models of lupus lacking the cytokine produce fewer auto-antibodies and have less severe renal disease.
The research team from Penn State Milton S. Hershey Medical Center studied mice that spontaneously develop autoreactive B-cells and auto-antibodies. For the purpose of the study, mice were specifically engineered to lack the interferon receptor only in B-cells. The team noted that in these animals, autoreactive B-cells did not form and there were lower levels of lupus auto-antibodies. In contrast, the absence of the interferon receptor did not affect the production of immune cells to foreign threats.
The study, “IFN-γ receptor and STAT1 signaling in B-cells are central to spontaneous germinal center formation and autoimmunity,” was led by Dr. Ziaur S.M. Rahman, assistant professor of microbiology and immunology at Penn State, and performed in collaboration with the Tokyo University of Science.
“This suggests that interferon gamma signaling in B-cells is critical for the formation of spontaneously developed B-lymphocyte groups and autoimmunity,” Rahman said in a press release. “If you could target this interferon gamma signaling pathway in B-cells, you could potentially treat lupus.”
Currently, lupus is treated with immuno-suppressive drugs, significantly increasing the risk for infections. Targeting the formation of autoreactive B-cells could offer a more selective treatment approach, not altering the body’s defense against pathogens.




