Researchers Discover a New Trigger for Autoimmune Diseases
Written by |
A team led by researchers at Garvan Institute of Medical Research and St. Vincent’s Clinical School in Australia identified a new trigger for autoimmune diseases. The study was recently published in the journal Immunity and is entitled “FAS Inactivation Releases Unconventional Germinal Center B Cells that Escape Antigen Control and Drive IgE and Autoantibody Production.”
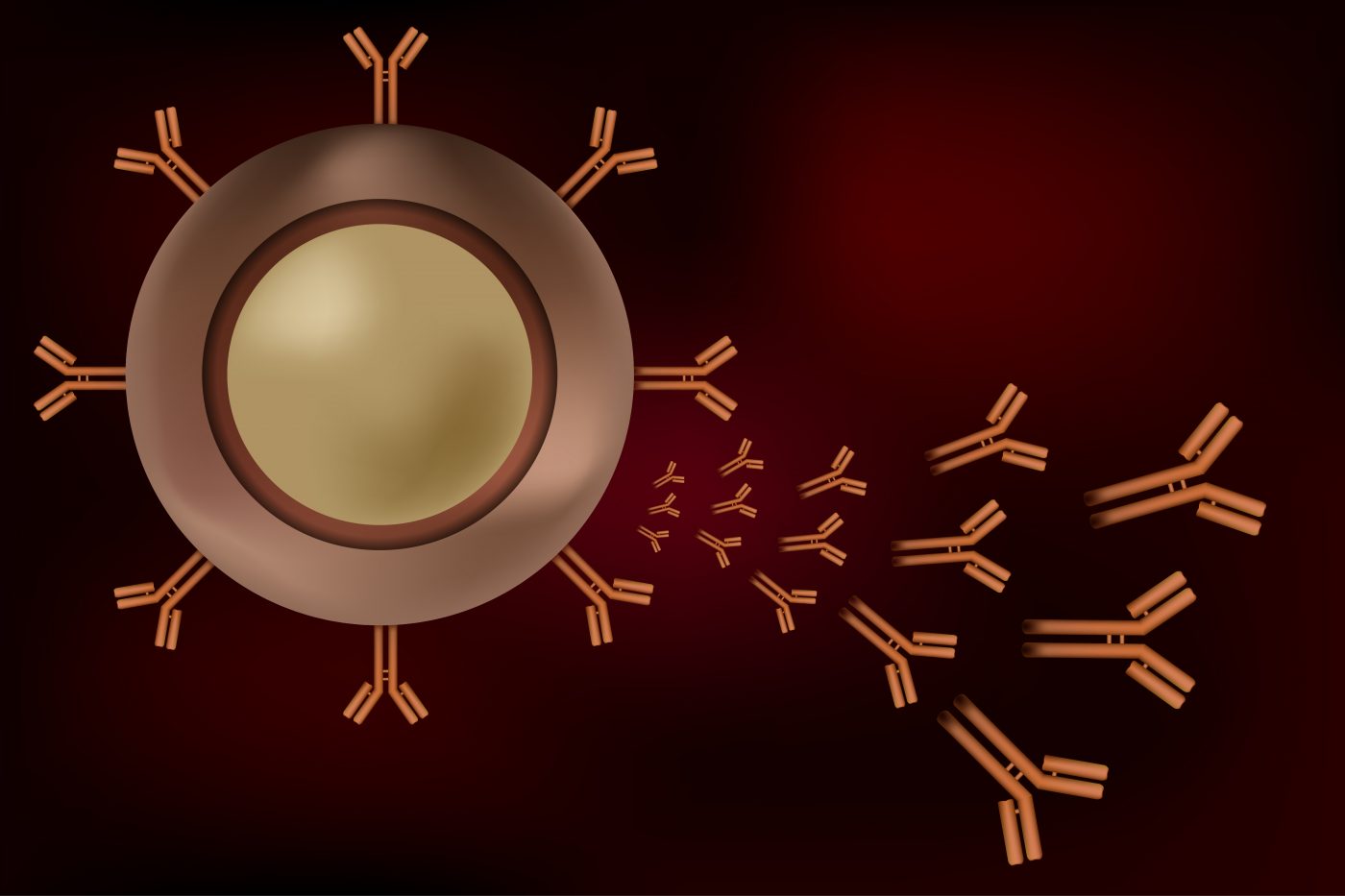
When a person develops an infection or is vaccinated, the body creates antibodies that are able to attack foreign microbes. In the case of autoimmune diseases like lupus, there is an overreaction of the body’s immune system and the antibodies produced attack the person’s own healthy tissues (autoantibodies), causing inflammation, pain, disability and often tissue destruction. The causes underlying autoimmune diseases are poorly understood, but genetic factors are thought to play a role. The link between autoantibody generation and genetic variation is, however, not clear.
It has been suggested that a gene called FAS is involved in preventing the formation of autoantibodies. This gene encodes a receptor that leads to programmed cell death, also known as apoptosis, resulting in the destruction of autoantibody-producing cells.
Researchers have now discovered that mutations in the FAS gene that allow the development of an unconventional subset of “rogue germinal center B cells,” which generate large numbers of cells that produce harmful antibodies, including autoantibodies. These rogue self-reactive cells develop in germinal centers, central factories where B lymphocytes (a type of white blood cell) proliferate, differentiate and set their antibody genes during a normal immune response.
The team believes that FAS plays a crucial role in preventing autoantibody production. “In very simple terms, we believe FAS prevents rogue germinal center B cells from developing, and we suspect that is its primary role,” said the study’s senior author Dr. Robert Brink in a news release.
“When we removed FAS from a mouse model, we saw the appearance of rogue cells in the germinal center,” explained Dr. Brink. “A disproportionately large number of plasma cells were formed by these rogue cells, producing antibodies you wouldn’t expect to see, very high numbers of IgE antibodies in particular. Instead of getting better at binding foreign antigen, rogue cells got worse — the opposite of what is supposed to happen in the germinal center! Most significantly, many of the antibodies derived from rogue cells turned out to be autoantibodies.”
Mutations in the FAS gene are known to cause an autoimmune disease called autoimmune lymphoproliferative syndrome (ALPS), a rare genetic disorder characterized by an abnormally high production of immune lymphocytes leading to their accumulation in the lymph nodes, liver and spleen, causing an enlargement of the organs. The research team analyzed data from ALPS patients and found that more than 25% of them had abnormally high blood levels of IgE antibodies, confirming their observations in mice.
Apart from ALPS, “High levels of IgE antibodies are being found in other autoimmune diseases, such as lupus, and IgE is becoming increasingly associated with severe disease,” noted Dr. Brink. “The fact that these rogue cells produce both autoantibodies and IgE antibodies, provides a compelling association with the more severe forms of autoimmunity.”
The team believes that these newly discovered “rogue germinal center B cells” are a major driver of autoantibody production and triggers of autoimmune disease.
“We do not yet know how rogue B cells arise — mutation of FAS is certainly one way, but there are likely to be others. Defining these mechanisms promises to advance our understanding of the genesis of autoimmune disease and will point the way towards new diagnosis and treatment strategies,” concluded Dr. Brink.