Levels of Specific Antibodies Linked to Clinical Characteristics of Lupus, Study Reports
Written by |
Levels of certain antibodies are significantly associated with particular clinical characteristics of systemic lupus erythematosus (SLE), and could be used to assess disease activity in patients, a study finds.
The study, “Antibodies to extractable nuclear antigens (ENAS) in systemic lupus erythematosus patients: correlations with clinical manifestations and disease activity,” was published in the journal Reumatismo.
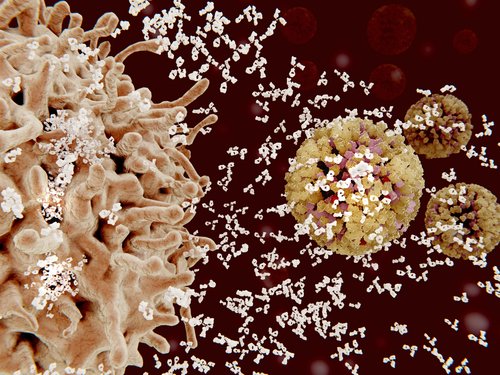
Lupus is an autoimmune disease characterized by high levels of antibodies that attack the body’s own tissue — known as autoantibodies.
Because these autoantibodies contribute directly to the mechanisms involved in the development of lupus, they are thought to appear either before the onset of the disease or along with it.
Anti-extractable nuclear antigen (anti-ENA) is one of the autoantibodies present in lupus patients. These are autoantibodies in the blood that react with proteins in the cell’s nucleus.
In lupus patients, the primary protein targets of anti-ENA include U1-ribonucleoproteins (RNP), Smith antigen (Sm), topoisomerase I, Jo-1, Ro (SS-A), and La (SS-B). These proteins, which reside in the nucleus, play major roles in gene expression.
Autoantibodies against ENA are typically present several years prior to a lupus diagnosis — before patients are exhibiting symptoms. However, the relationship between lupus disease activity and levels of anti-ENA is not well-known.
Researchers in this study set out to explore the correlations between anti-ENA and clinical characteristics and disease activity in lupus patients.
They analyzed 70 SLE patients, 64 of whom were female. They assessed disease activity using both the SLE activity index (SLEDAI) and the British Isles Lupus Assessment Group (BILAG).
The presence of anti-Ro/SSA antibodies positively correlated with headaches, blurred vision, and SLEDAI score, indicating that patients with high levels of anti-Ro/SSA antibodies were more likely to have higher disease activity.
Anti-La/SSB also positively correlated with headaches and SLEDAI, meaning that high levels of anti-La/SSB were also indicative of worse disease activity.
Anti-Sm antibodies correlated positively with disease duration, 24-hour urinary proteins (indicative of impaired kidney function), SLEDAI score, and BILAG renal score.
Patients with high levels of anti-dsDNA were more likely to have a higher BILAG renal score, SLEDAI score, 24-hour urinary proteins, and ESR, a test that measures the degree of inflammation.
One of the major complications of SLE, lupus nephritis, or inflammation of the kidney, was significantly correlated with anti-dsDNA levels and anti-Sm antibodies.
These results indicate that anti-ENAs — including anti-Ro/SSA, anti-LA/SSB, anti-Sm, and anti-dsDNA — are significantly associated with various clinical characteristics of lupus patients, and could potentially play a role in assessing disease activity.
“Insight into these ENAs may lead to new approaches to diagnostic testing, accurate evaluation of disease activity and lead to target approach for SLE,” the researchers said.




