OX40L-Positive B-Cells Are Key Players in Lupus Autoimmunity, Study Finds
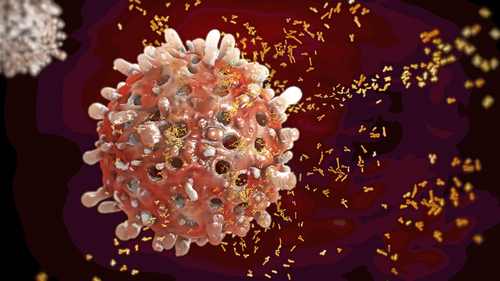
The protein OX40L, produced by immune B-cells, plays a key role in the development of systemic lupus erythematosus (SLE) by activating a T-cell subset involved in autoimmunity, new research has found.
Inhibition of OX40L B-cells improved lupus symptoms in mice, suggesting that OX40L is a promising new target for lupus treatment.
The study, “B cell OX40L supports T follicular helper cell development and contributes to SLE pathogenesis,” was published in the journal Annals of the Rheumatic Diseases.
Lupus is a chronic autoimmune disease characterized by the production of antibodies against nuclear proteins. Similar to most other autoimmune disorders, the risk of lupus is influenced by environmental and genetic factors. Among the 50 genes affecting the risk for lupus is TNFSF4, the gene that codes for OX40L.
OX40L is a costimulatory molecule found at the surface of many cell types, including dendritic cells, B-cells, macrophages, activated T-cells, and endothelial cells — the cells lining blood vessels. Its receptor, on the other hand, is mainly produced by a subset of T-cells, called follicular helper T-cells, or CD4 T-cells.
While this signaling pathway is known to be involved in multiple immune response mechanisms, it was unclear how OX40L could actively contribute to lupus development.
In an attempt to assess which OX40L-expressing cell types were mediating lupus risk, researchers at King’s College London and Imperial College London conducted a series of experiments on lupus animal models. The team developed genetically engineered animals that did not express OX40L in their B-cells or their T-cells.
The strategy allowed them to identify OX40L expressing B-cells as the key elements mediating lupus symptoms. In the absence of these cells, mice had improved lupus symptoms, which was accompanied by a reduction in autoantibodies and their deposition in the kidneys.
Further experiments revealed that OX40L B-cells were necessary to mediate immune responses known to be involved in autoantibody production and overactive immune responses.
“These findings contribute to a model in which genetically determined increased OX40L expression promotes human SLE by several mechanisms, contingent on its cellular expression,” the study concludes. “The improvement in pathology in two models of systemic autoimmunity indicates that OX40L is an excellent therapeutic target in SLE.”






