Lupus Eye Damage May Provide a Window Into Disease Activity
Written by |
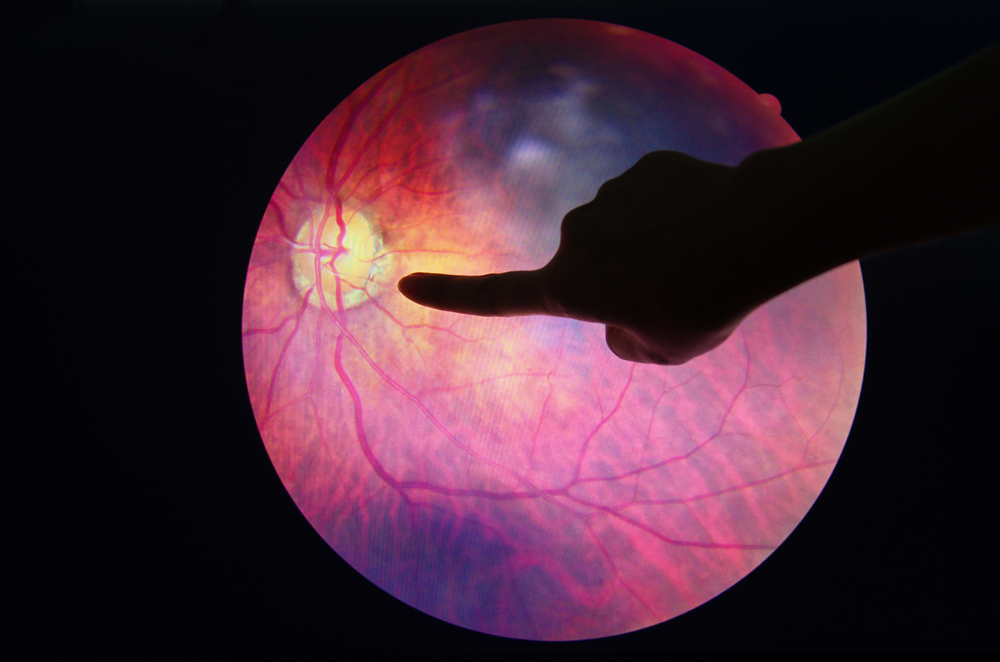
Eye damage, also referred to as retinopathy, caused by systemic lupus erythematosus may be a sign of more severe disease, as patients with lupus retinopathy have kidney damage more often than patients without eye disease.
As lupus retinopathy is suggested to reflect damage to small blood vessels throughout the body, researchers suggested that regular eye examinations should be used to monitor disease progress, particularly because changes in damage to the retina may signal the advent of a disease flare.
The study, “Role of lupus retinopathy in systemic lupus erythematosus,” was published in the Journal of Ophthalmic Inflammation and Infection.
Researchers at Tribhuvan University Institute of Medicine in Nepal recruited 91 lupus patients for the study, with the aim to compare symptoms and laboratory measures between patients with and without eye damage.
The research team found retinopathy in 11 patients (12.1%), nine of whom had one eye affected, and two had damage in both eyes. The average age did not differ between patients with and without retinopathy.
The majority of the examined eyes (61.5%) showed mild damage, while 15.4% were moderately damaged, and 23.1% were severely affected. In the severe cases, researchers found retinal vasculitis — an inflammation of the small blood vessels in the retina — as well as blocked blood vessels.
Kidney disease was more common among patients with retinopathy than among those without the condition. In fact, all 11 patients with retinopathy had kidney involvement, compared to 59.3% in patients without eye damage. This was mirrored in the higher levels of serum creatinine (a marker of kidney function; high levels mean the kidneys are not working properly) among patients with eye disease.
Central nervous system conditions (namely chorea, convulsion, and epilepsy) also were more common among patients with retinopathy — 27.3% compared to 11% — but the difference was not statistically significant. Although the levels of the characteristic lupus autoantibodies antinuclear (ANA), anti-dsDNA, and antiphospholipid antibodies tended to be higher in patients with eye disease, the differences were again not significant.
Based on the results, researchers suggest that ophthalmologists should be part of a multidisciplinary team managing lupus patients, to gain a better understanding of disease status and to allow more accurate treatment decisions.




