Stroke Risk in SLE Patients May Be Linked to Cerebral Small Vessel Disease, Study Finds
Written by |
A case-control study found that patients with systemic lupus erythematosus (SLE) show a high prevalence of brain alterations that are clinically associated with cerebral small vessel disease (SVD) — a potential cause of strokes — although a clear link between SLE and SVD was not established.
SLE is an inflammatory autoimmune disease that can involve the brain, and SLE patients are known to be at greater risk for strokes, but the reasons for this risk are unclear.
One hypothesis is that systemic inflammation in the brain can damage cerebral small vessels, eventuallying lead to cerebral SVD. That condition is characterized by cognitive impairment and dementia, depression, and balance problems.
In the study, “Cerebral Small Vessel Disease Burden Is Increased in Systemic Lupus Erythematosus,” published in the journal Stroke, researchers compared several well-established biomarkers of cerebral SVD in SLE patients and control healthy subjects, or to patients who suffered a minor stroke event, to better understand the mechanism responsible for the increased stroke risk in SLE patients.
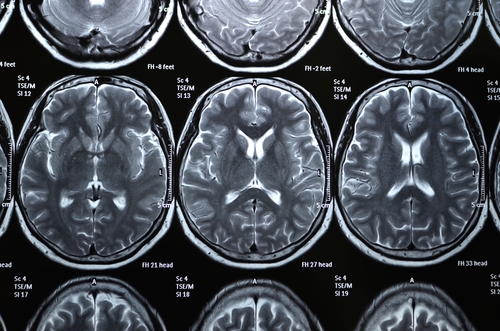
Brain magnetic resonance imaging (MRI) analysis showed that the majority of the SLE patients presented brain structure alterations, as visible perivascular spaces (PVS, cerebrospinal fluid-filled spaces around blood vessels) and white matter hyperintensities (WMHs, brain areas with lesions).
Comparing these imaging results, the researchers determined that SLE patients had higher SVD scores than those in the control and stroke groups. Specifically, SLE patients showed higher PVS and WMHs scores, and more superficial brain atrophy, than healthy controls. Compared with stroke patients, those with SLE presented more PVS and an equal WMH burden, despite the SLE patients being slightly younger than those with strokes, and having fewer vascular risk factors like smoking.
Although most SLE patients showed features of cerebral SVD, the researchers could not associate the total SVD score with SLE activity, cognition, disease duration, or any blood measure.
“The higher burden of PVS in SLE patients, in the absence of vascular risk factors, is consistent with the known association between PVS and plasma markers of inflammation in patients with SVD and suggests that inflammation may be associated with subclinical microvascular brain damage in SLE patients,” the researchers concluded.
Further studies are needed into the importance and involvement of cerebral SVD in SLE, they said. It is particularly necessary to understand the impact that SLE activity and disease treatments, as well as patient diet and lifestyle, may have in causing or accelerating brain damage in these people.




