Mouse Study Links Lupus-Like Disease to an Inability to Digest and Clear Body of Dead Cells
Defects that disrupt the digestion of dead cells can result in a lupus-like autoimmune disorder, according to a study titled “Noncanonical autophagy inhibits the autoinflammatory, lupus-like response to dying cells” and recently published in the journal Nature by scientists at St. Jude Children’s Research Hospital.
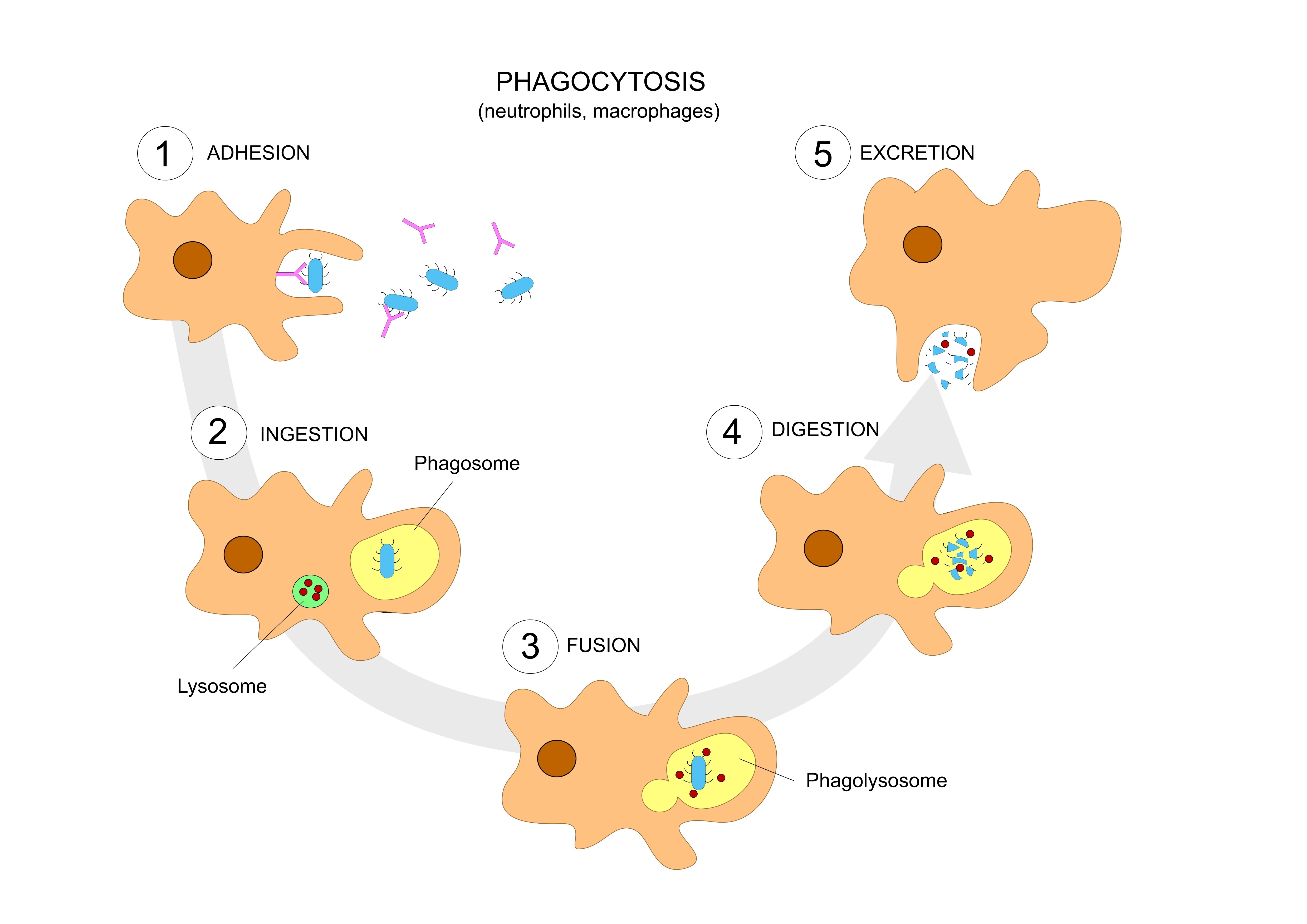
Research has previously shown that a form of noncanonical autophagy, known as LC3-associated phagocytosis (LAP), is important to the correct disposal of dead and dying cells after their digestion by macrophages, a type of immune cell. These observations led to the findings that mice with a LAP defect are significantly smaller than those without the defect, and have increased levels of inflammatory cytokines and autoantibodies (i.e., antibodies produced by the immune system that are directed against the body’s own proteins). These mice also showed organ damage, specifically in the kidney, a phenotype associated with systemic lupus erythematosus (SLE). Notably, these alterations were only associated with LAP defects, and not other types of authophagy (cell digestion) defects.
To investigate the role of LAP in SLE in vivo, researchers injected LAP-deficient mice with dying cells, observing that macrophages could effectively engulf these cells. Their digestion, however, was less efficient and triggered a rapid increase in pro-inflammatory cytokines, while the anti-inflammatory interleukin (IL)-10 decreased. Repeat injections of dying cells enhanced this pro-inflammatory phenotype of lupus-like illness in the LAP-deficient mice, while increasing the levels of autoantibodies. Once again, none of the lupus-associated phenotypes were observed in mice with defects in conventional autophagy.
“Defects in the clearance of dying cells have been implicated in the SLE disease process, and previous studies have suggested that the problem may stem from defects in autophagy,” Douglas Green, PhD, a St. Jude Department of Immunology chair and study lead author, said in a press release.
“In this study, we showed that LAP contributes to SLE in mice and likely accounts for the previously reported genetic association between autophagy and lupus,” he added.
“We hope the findings offer a window into the cause of this devastating disease in some patients, and an opportunity to improve treatment by developing novel approaches to prevent or reduce the inflammation and autoimmune response that characterize lupus,” Dr. Green concluded.





