PAH an Important Prognostic Factor in Lupus Patients, According to Review
Written by |
Pulmonary arterial hypertension (PAH) is a prevalent comorbid factor in systemic lupus erythematosus (SLE) patients, significantly increasing mortality outcomes. This is the conclusion of a recent review titled “Survival and prognostic factors of systemic lupus erythematosus-associated pulmonary arterial hypertension: A PRISMA-compliant systematic review and meta-analysis,” published in the journal Autoimmunity Reviews.
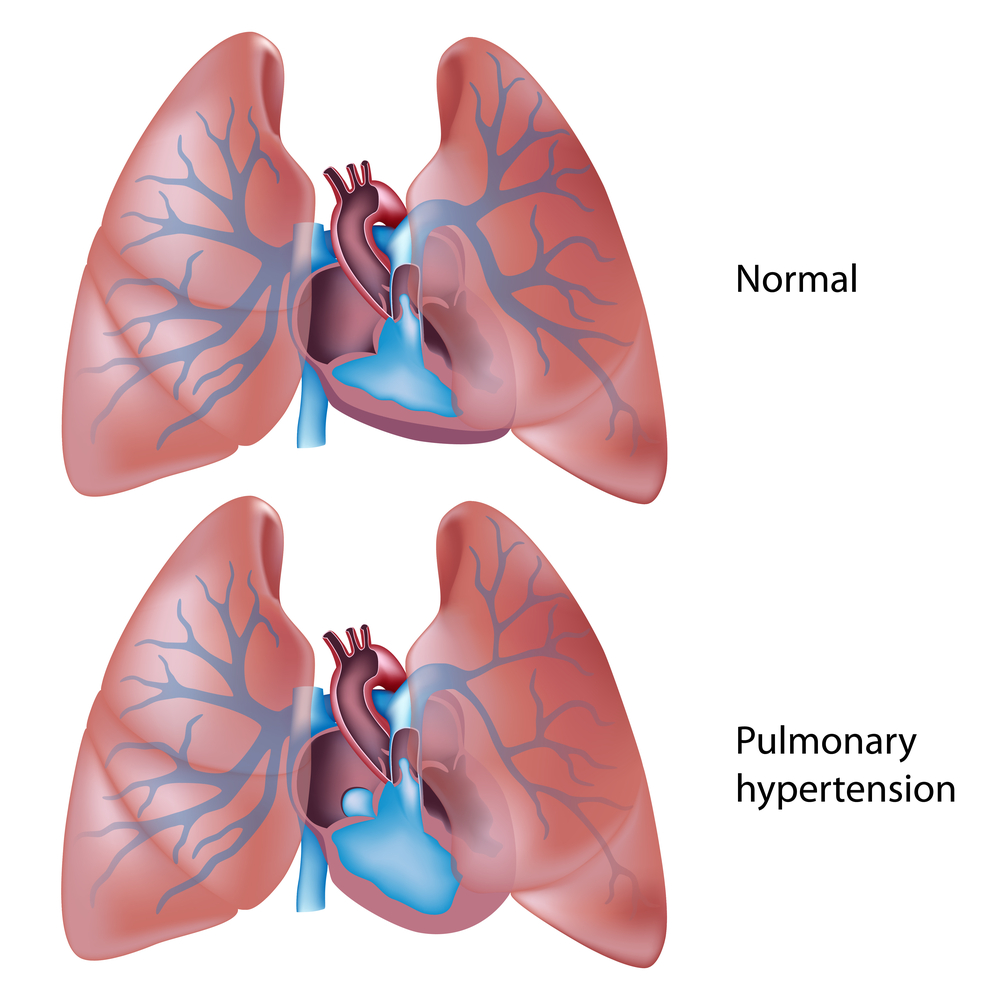
PAH is defined as a mean pulmonary arterial pressure greater or equal to 25 mmHg at rest. Previous reports have suggested that pulmonary arterial hypertension is an independent prognostic factor and the third leading cause of mortality in patients with SLE, largely due to right heart failure with circulatory collapse and superimposed respiratory failure.
The review’s authors performed a systematic review and meta-analysis of published literature to determine the rate of survival of patients with SLE-associated PAH. They searched MEDLINE (OVID), EMBASE, Cochrane Central Register of Controlled Trial, and Scopus databases and identified 892 articles. After duplicates were removed and thoroughly screened, the team included six studies for the meta-analysis, which encompassed a total of 323 patients with SLE-associated PAH, according to the inclusion and exclusion criteria.
The meta-analysis showed that the pooled one, three, and five-year survival rates of SLE-associated PAH were 88 percent, 81 percent, and 68 percent, respectively. The detrimental effect of PAH in these patients was noted when comparing both the 5-year and 10-year survival rates of patients with only SLE, which were 92 percent to 94 percent, and 88 percent to 91 percent, respectively.
These results show there is a significant impact on patients’ survival when they are affected with PAH. Moreover, WHO Functional class (Fc) III/IV (a functional classification system for PAH patients) is an independent prognostic factor of mortality in this patient population, along with other factors also associated with poor survival, including higher mean pulmonary arterial pressure (mPAP), higher pulmonary vascular resistance (PVR), lower six minutes walking distance (6MWD), higher brain natriuretic peptide (BNP) and higher N-terminal proBNP (NT-proBNP) levels.
The authors conclude there is a poor long-term survival prognosis of SLE-associated PAH patients, but stress that early diagnosis and management are important to increase survival outcomes.





