Diffuse Alveolar Haemorrhage Reduces SLE Patients’ Long-term Survival
In a recent study entitled “Systemic lupus erythematosus complicated by diffuse alveolar haemorrhage: risk factors, therapy and survival” researchers performed the first study investigating the risk factors for diffuse alveolar haemorrhage in systemic lupus erythematosus and how it impacts patients’ therapy responses and outcomes. The study was published in the LUPUS Science & Medicine journal.
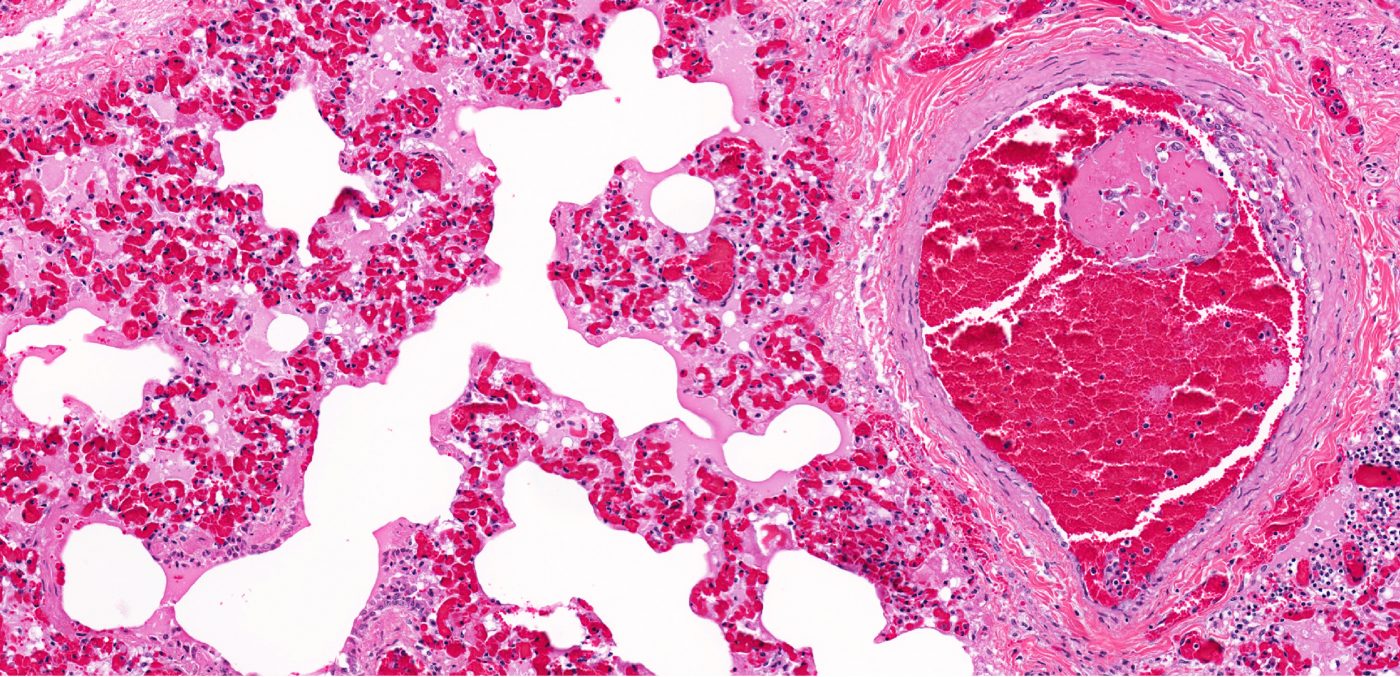
Diffuse alveolar haemorrhage (DAH) is a severe and life-threatening complication of systemic lupus erythematosus (SLE), estimated to affect between 2 to 5% of SLE patients. DAH is characterized by symptoms of pulmonary haemorrhage (denoted by bloody bronchoscopy accompanied by dyspnea and coughing of blood); drop in haemoglobin and immune cellular infiltrates into the chest. However, despite its severity the risk factors and patients responses to DAH treatments remains poorly understood.
In this study, the authors describe 22 cases of DAH-associated lupus using the Michigan Lupus Cohort with approximately 1,000 patients. Patients were considered DAH positive if they presented three criteria: at least one sign of pulmonary haemorrhage (either dyspnoea, cough, haemoptysis, hypoxaemia or bloody bronchoscopy), haemoglobin drop below 1.5 g/dL and pattern of immune cellular infiltrates by chest X-ray or chest CT scan. Patients with confirmed DAH were compared to 66 patients from the same outpatient cohort.
The researchers observed that 59% of DAH patients were diagnosed within five years after their lupus diagnosis. A link between DAH and antiphospholipid syndrome (APS) had been previously reported, with authors now finding an increase in manifestation of both DAH and APS, an autoimmune disorder, in SLE patients. The team noted that a history of both leucopenia (a reduction in the number of white cells in the blood) and thrombocytopenia (deficiency of platelets in the blood) were two factors strongly associated with DAH. Particularly, they found that thrombocytopenia was the key predictor of DAH in the cohort of patients and, together with a history of low complement C3 were the two risk factors for DAH.
DAH patients’ treatment strategy was based on immunosuppressants, including combinations of corticosteroids, plasmapheresis, cyclophosphamide, rituximab and mycophenolate mofetil. However, despite a good initial response, these patients’ long-term survival was significantly reduced when compared to lupus patients without DAH. Furthermore, the majority of deaths were due to thrombotic complications.






