Blisibimod: Potential Treatment for Systemic Lupus Erythematosus
In a new study entitled “Treatment of systemic lupus erythematosus patients with the BAFF antagonist “peptibody” blisibimod (AMG 623/A-623): results from randomized, double-blind phase 1a and phase 1b trials” authors determined the safety, tolerability and efficacy of blisibimod, a B cell-activating factor antagonist, in patients with systemic lupus erythematosus. The study was published in the journal Arthritis Research & Therapy.
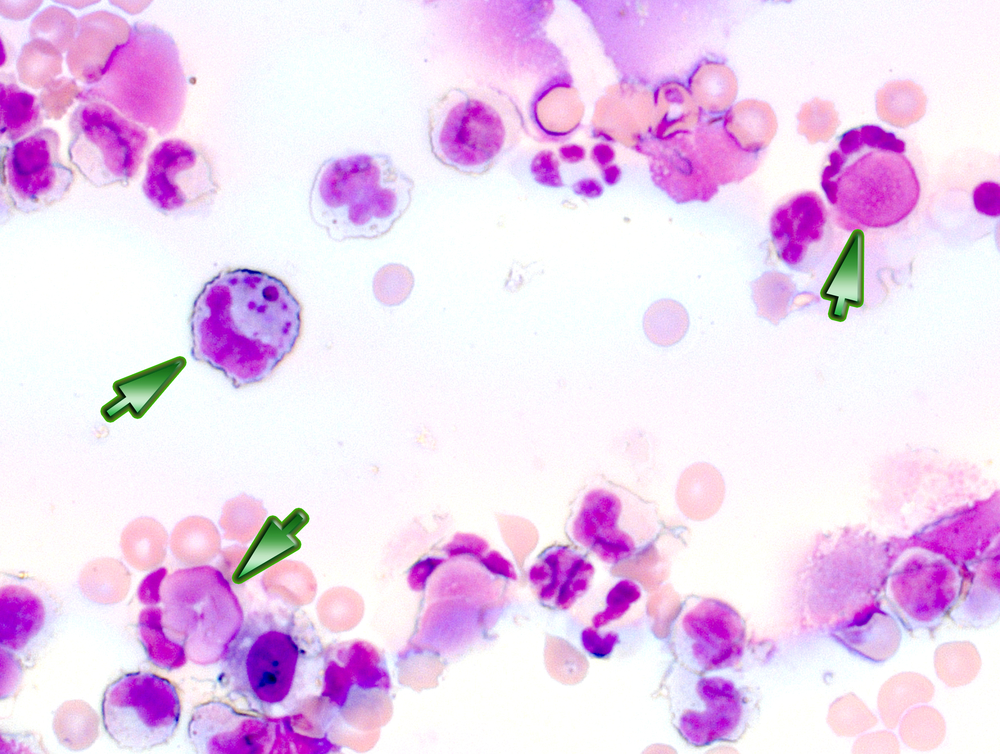
Systemic lupus erythematosus (SLE) is an autoimmune disease and the most common type of lupus. Despite presenting a heterogeneous clinical and immunologic profile, the common underlying triggering factor across patients is the hyperactivity of B cells – key cells of the immune system responsible for producing antibodies, that when mistakenly attack the body’s own cells lead to SLE development. Therefore, targeting B cells is considered a major therapeutic intervention against SLE.
B cell-activating factor (BAFF) is critical for B cells’ survival and differentiation, with studies on SLE animal models showing that BAFF overexpression promotes features of SLE, while targeting BAFF attenuates SLE progression. The same pattern has been observed in SLE human patients, with 50% of patients presenting increased circulating levels of BAFF, with disease severity correlating to its increase.
Researchers performed two multicenter, double blind, placebo-controlled trials where they assessed the safety, tolerability, pharmacokinetic and pharmacodynamic profiles of blisibimod – a BAFF antagonist, which binds both membrane-bound and soluble BAFF – in SLE patients. To this end, the team enrolled SLE patients (either men or women with 18 to 65 years of age, diagnosed with SLE for at least 1 year) with disease at an inactive or stable state. SLE patients received either a single dose of blisibimod (subcutaneously at 0.1, 0.3, 1, or 3 mg/kg or intravenously at 1, 3, or 6 mg/kg) and were compared to placebo control SLE patients. At a second phase, patients were treated with four weekly doses of blisibimod (0.3, 1, or 3 mg/kg subcutaneously or 6 mg/kg intravenously) and compared with the same regimen in the placebo group.
The diagnosis of SLE for more than 1 year was confirmed in 93% females where the team observed that single- and multiple-dose treatment with blisibimod resulted in a significant decrease in the number of B cells (from 24 to 76%) and B cell surface molecule density. Of note, blisibimod treatment produced no notable changes in other cells of the immune system, including T cells or natural killer cells. The results were consist and linear between the two administration routes, either subcutaneous or intravenous. When compared to the placebo control arm, blisibimod exhibited a similar safety and tolerability profile and was well tolerated.
Hence, authors highlight that these findings support the use of BAFF antagonists, such as blisibimod as a potential new treatment for SLE and other B cell-mediated diseases. This should be evaluated in future larger clinical trials.






