Targeting T-cell Exhaustion As a Therapy For Lupus Patients
In a new study entitled “T-cell exhaustion, co-stimulation and clinical outcome in autoimmunity and infection” researchers discovered how T-cell exhaustion can determine the outcome of autoimmune diseases, suggesting that therapeutics targeting the underlying mechanism of T-cell exhaustion can benefit patient outcomes in diseases like systemic lupus erythematosus. The study was published in the journal Nature.
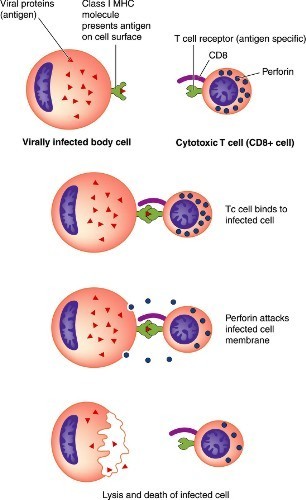
T cells are key players in the immune system, responsible for fighting infections and abnormal cells, such as cancer cells. However, while they play a crucial role in body defense, they can also lead to autoimmune diseases as a consequence of abnormally attacking our own healthy cells instead of foreign pathogens.
CD8+ T cells are a specific group of T cells that during a chronic infection can become ‘exhausted’ and therefore fail to protect against infections, resulting in persistent chronic viral infections such as those with hepatitis C or HIV. Nonetheless, T-cell exhaustion may be beneficial when considering autoimmune diseases.
In this study, researchers from the Cambridge Institute for Medical Research investigated the genetic profile of CD8 T-cells in autoimmune patients. They found that the gene expression signature was similar between autoimmune and chronic infected patients, suggesting that this mechanism actually impacts disease outcomes. Notably, while T cell exhaustion led infections to persist it had the exact opposite effect in autoinflammatory disorders: patients exhibited a mild-disease phenotype accompanied with fewer relapses.
As Dr Eoin McKinney, a Wellcome Trust-Beit Research Fellow at the University of Cambridge and study first author explained, “We know that the way our bodies respond to infection and to autoimmune diseases differs between individuals. In part, we believe this is due to a process known as T cell exhaustion. For effective treatment, we need to exhaust our T cell responses in autoimmune diseases — and hence limit the attack on our body — and to reverse exhaustion when the fight is against unwanted invaders, such as viruses or cancer.”
The team highlighted how their findings may help clinicians allocate effective treatments to patients suffering with autoimmune diseases, depending on their T cells exhaustion status: patients with a higher level of exhausted T cells have a better long-term outcome and therefore require less intensive therapy, while those with ‘non-exhausted’ T cells may benefit from more intensive treatments. This approach is currently being tested in a clinical trial, commissioned by the same team, on inflammatory bowel disease patients.
Professor Ken Smith, study lead author added, “We believe the clinical implications of this study could be profound. A test based on the concept is soon to enter the clinic, and we are exploring new treatments for autoimmunity based on manipulating T cell exhaustion. A focus on T cell exhaustion in cancer has led to a revolution in treatment and a multi-billion dollar industry. We now implicate the same pathways in determining long term patient outcome in autoimmune and inflammatory diseases, which afflict up to one in ten of the population over the course of their lives.”






