Testing for Antibodies Against p40 May Help Diagnose Lupus Earlier, Study Shows
Systemic lupus erythematous patients with antibodies against the protein LINE-1 p40 are more likely to have active and severe disease, a study shows.
Since the presence of antibodies against p40 likely represents an early immune response, testing for it may help diagnose the disease earlier on, researchers say.
The study, “High prevalence and disease correlation of autoantibodies against p40 encoded by long interspersed nuclear elements (LINE‐1) in systemic lupus erythematosus,” was published in the journal Arthritis & Rheumatology.
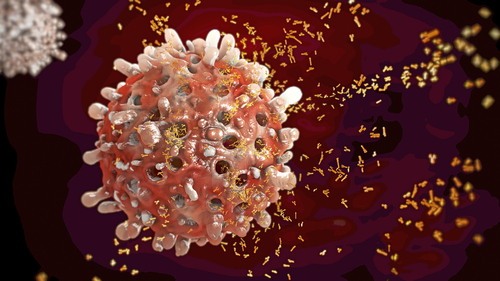
Systemic lupus erythematous (SLE) is an autoimmune disease, which means that it develops as a result of the immune system attacking healthy tissues in the body.
Patients with SLE have have antibodies that are directed toward the normal proteins in the body, which are known as autoantibodies.
Line scattered nuclear elements (LINE-1) is a segment of DNA that makes up about 17% of the human genetic material. In particular, the LINE-1 DNA segment provides instructions to cells to make two proteins, known as p40 and ORF2p.
These two proteins have been shown to assemble together with some well-known autoantigens — proteins that cause autoimmune reaction — in people with SLE. Therefore, researchers sought to determine whether SLE patients also make autoantibodies against p40.
First, the researchers quantified the amount of p40 autoantibodies that were present in the serum — a component of blood — of SLE patients, healthy people, and those with systemic sclerosis, another autoimmune disease.
Results indicated that autoantibodies against p40 were present in a majority of patients and many healthy controls. However, levels of p40 autoantibodies were significantly higher in people with SLE compared with both healthy controls and systemic sclerosis patients.
Next, researchers looked at levels of p40 autoantibodies in people with SLE with different levels of severity. They found that anti-p40 reactivity was higher in patients during a flare compared with that of people in remission.
The findings showed that — consistently — p40 autoantibody levels significantly correlated with SLEDAI, a validated measure of SLE disease activity. That further indicated that p40 autoantibodies are present in people with more severe disease.
p40 antibody levels also correlated with other markers of disease activity and severity, such as type I interferon score, complement C3 decrease, anti-DNA antibodies. and anti C1q antibodies. All of these are indicators of inflammatory autoimmune activity.
People with higher p40 antibody levels also were more likely to have a current or past history of nephritis, or inflammation of the kidneys.
In totality, the findings suggest that “autoantibodies reacting with LINE‐1 p40 characterize a population of SLE patients with severe and active disease,” the researchers said.
Finally, researchers showed that, in addition to antibodies against p40, people with SLE also had antibodies against p40-associated proteins.
“Autoantibodies reacting with LINE‐1 p40 characterize a population of SLE patients with severe and active disease,” the investigators said.
“These autoantibodies may represent an early immune response against LINE‐1 p40 that does not yet by itself imply clinically significant autoimmunity, but may represent an early, and still reversible, step towards SLE pathogenesis,” they added.
Therefore, testing for these antibodies may help diagnose SLE at an early stage and even help prevent lupus progression, the researchers said.





