Targeting cGAS-STING Pathway Might Help Identify Lupus Therapies
Designing therapeutics that block cGAS–STING — a cell-signaling pathway associated with inflammation — could help treat patients with systemic lupus erythematosus, a new study suggests.
The study, “Apoptosis-derived membrane vesicles drive the cGAS–STING pathway and enhance type I IFN production in systemic lupus erythematosus,” was published in the journal Annals of the Rheumatic Disease.
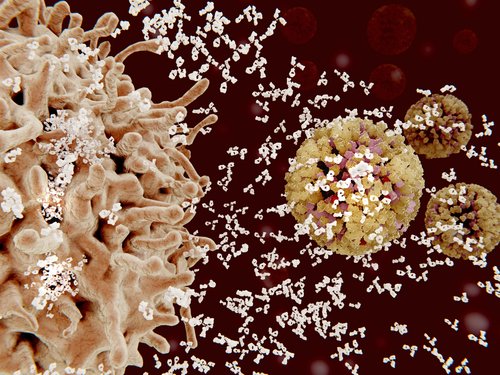
Systemic lupus erythematosus (SLE) is an autoimmune disease in which antibodies are produced against a patient’s own tissues. Specifically, SLE patients have high levels of autoantibodies (self-antibodies) against nucleic acids, such as DNA, and the proteins that interact with DNA.
While the exact reason for SLE development is not known, researchers know that type I interferon (IFN-I) plays a very important role in SLE. Type I interferons are a large group of proteins that help regulate the activity of the immune system by activating expression of genes involved in inflammation.
Levels of IFN-I and of several IFN-I-stimulated genes (ISGs) are elevated in patients with SLE and associated with SLE disease activity. In fact, clinical lupus actually can develop after long-term treatment of patients with chronic hepatitis with IFN-α (a kind of type I interferon).
IFN-I proteins are produced by activation of pattern-recognition receptors (PRRs), which, as the name implies, are activated upon recognition of specific patterns, such as the patterns of DNA.
PPR proteins that recognize DNA are crucial for the onset of SLE. Among them are the toll-like receptor 9 (TLR9) and cyclic GMP–AMP synthase (cGAS)–stimulator of interferon genes (STING).
It is known that stimulation of TLR9 by DNA and immune complexes from patients with SLE leads to excess production of IFN-I. While TLR9 is important for SLE development, there are other mechanisms that contribute to IFN-I production.
Given that cGAS and STING also are involved in DNA recognition, the cGAS–STING pathway may play a role in SLE.
So, researchers set out to investigate the role of the cGAS–STING pathway in SLE. They collected serum samples from patients with SLE, patients with other autoimmune diseases, and healthy controls, and looked for levels of IFN-I and IFN-I-stimulated genes.
As expected, IFN-I activity and levels of IFN-I-stimulated genes were higher in patients with SLE than in patients with other autoimmune diseases or healthy controls.
Researchers also used cells that lacked the cGAS and STING pathways to study the levels of IFN-I-stimulated genes of these cells.
Interestingly, STING-depleted cells had lower levels of IFN-I-stimulated genes, indicating that STING plays a major role in carrying out IFN-I activities. Consequently, STING-dependent stimulation of IFN-I-stimulated genes correlated with disease activity.
While DNA levels were higher in SLE patients, researchers found that cell-free DNA was not causing an increase in IFN-I-stimulated genes. Thus, they tested a kind of extracellular vesicles that form when a cell dies.
These vesicles, called apoptosis-derived membrane vesicles (AdMVs), isolated from SLE patients, had the ability to increase IFN-I-associated genes. And this activity was reduced in cGAS-depleted or STING-depleted cells.
“These results indicate that AdMVs in SLE serum promote IFN-I production and ISG induction through the cGAS–STING pathway,” researchers explained.
Essentially, these results suggest that blocking the cGAS–STING pathway represents a promising therapeutic target for SLE.





