Antibody Reduces Inflammation, Skin Lesions in SLE Patients, Trial Shows
BIIB059, an antibody that targets a receptor of plasmacytoid dendritic cells, was well-tolerated and reduced inflammation and skin lesions in systemic lupus erythematosus (SLE) patients, a Phase 1 trial shows.
The study, “Monoclonal antibody targeting BDCA2 ameliorates skin lesions in systemic lupus erythematosus,” was published in The Journal of Clinical Investigation.
SLE is a chronic autoimmune disease characterized by excessive inflammation and tissue damage. Common symptoms include skin rash, arthritis, and nephritis (inflammation of the kidneys).
Current treatments for SLE include antimalarial drugs and corticosteroids, but these only partially treat the symptoms, and have negative side effects such as toxicity. Thus, new treatments for SLE are needed.
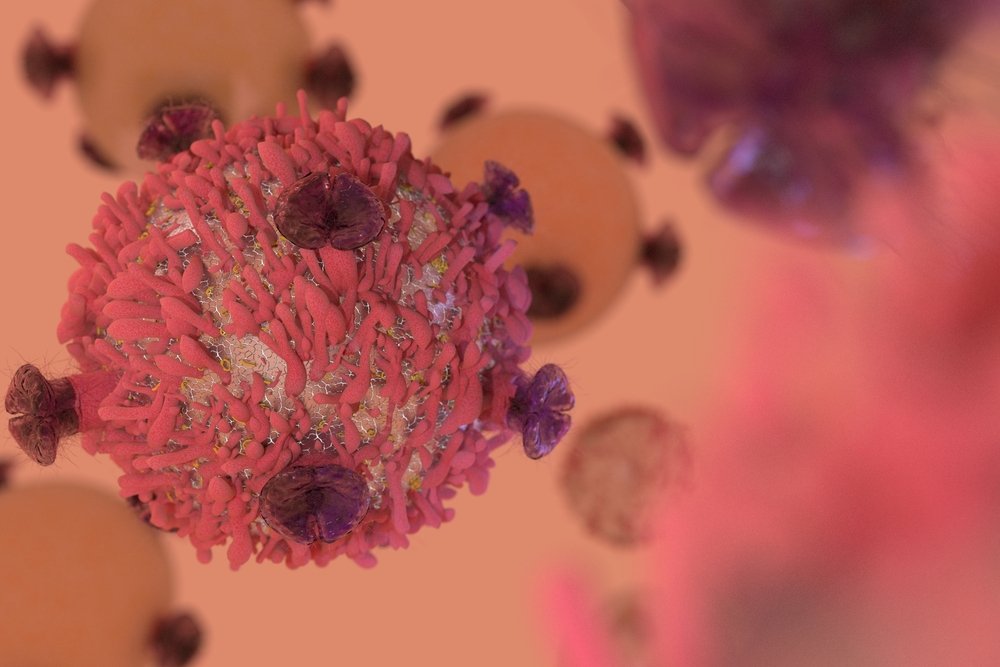
Plasmacytoid dendritic cells are immune cells that produce large amounts of type I interferon (IFN-I), an inflammatory molecule with a primary role in SLE progression. These cells migrate from the blood to affected tissues, where they cause increased inflammation and promote lesion formation. Therefore, they are an appealing target for SLE therapies.
BIIB059 is a humanized antibody — an antibody produced in another organism and engineered to be tolerated by humans — that binds BDCA2, a receptor specific to plasmacytoid dendritic cells. In preclinical studies, the antibody inhibited the production of IFN-I and other inflammatory molecules by these cells.
Thus, researchers conducted a Phase 1 trial (NCT02106897) to assess the safety, tolerability, pharmacokinetics (how substances move within the body), and pharmacodynamics (effects and action of substances within the body) of a single dose of BIIB059.
The trial had three parts. The first part evaluated the safety of increasing doses of BIIB059 on 54 healthy volunteers, from 18 to 55 years old. The second and third parts evaluated the effects of BIIB059 on 12 adult SLE patients that had mild to moderate skin lesions at the beginning of the study. Overall, 8 patients received the antibody, and 4 received the placebo.
Researchers measured the concentration of BIIB059 and IFN-I in blood and skin biopsies, and the amount of BDCA2 in plasmacytoid dendritic cells. The level of skin lesions was determined using the Cutaneous Lupus Erythematosus Disease Area and Severity Index Activity (CLASI-A).
Healthy volunteers and SLE patients showed good tolerance to all BIIB059 doses, and only experienced mild or moderate side effects. All participants finished the trial. The most common side effects were infections in the upper respiratory tract.
BIIB059 remained in the patient’s blood for about two weeks. During that time, plasmacytoid dendritic cells exposed very little BDCA2, and therefore did not produce IFN-I.
“Patients who received BIIB059 demonstrated a reduction of ~50% in (interferon-related genes) expression in whole blood 24 hours after administration,” the investigators wrote. Also, interferon-related protein expression was reduced by 70% in the skin lesions.
Of the 8 patients treated with BIIB059, 6 showed a reduction of at least 4 points in their CLASI-A scores — a measure of disease activity in the skin — four weeks after the therapy. Five of these patients maintained the response for 12 weeks. Patients who responded better were those that expressed less interferon-related genes.
In contrast, only 1 of the 4 patients in the placebo group showed an improvement in CLASI-A scores at weeks four and 12.
“BIIB059 is the first therapy to specifically target pDCs (plasmacytoid dendritic cells) in patients with SLE,” the researchers said.
“Our results highlight the central role of pDC-derived IFN-I in the pathogenesis of skin manifestations in SLE and suggest that targeting pDCs with BIIB059 is a promising therapy for SLE” and lupus cutaneous lesions, they stated.