Lupus Flares May Be Linked to Damage to Mitochondria, Study Reports
Excessive production of type I interferon (IFN-I) — a molecule that mediates immune and inflammatory responses — in people with systemic lupus erythematosus (SLE) may be caused by small fragments of mitochondrial DNA (mtDNA) that are released upon damage, a study suggested.
The study, “VDAC oligomers form mitochondrial pores to release mtDNA fragments and promote lupus-like disease,” was published in the journal Science.
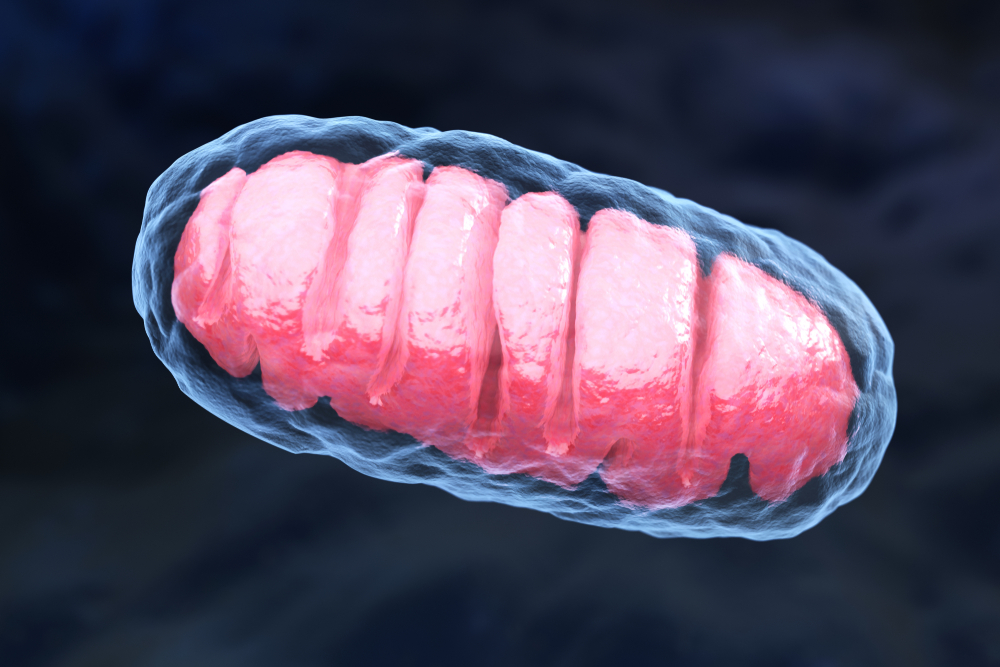
Mitochondria are the small compartments in cells that are responsible for producing cellular energy. When damaged, due to things like oxidative stress, for example, small bits of mtDNA may be released into the cytosol, the liquid-like substance that fills the interior of cells.
Oxidative stress refers to the damage to cells caused by high levels of oxidant molecules, or reactive oxygen species.
After reaching the cytosol, these small mtDNA fragments may activate certain immunostimulatory DNA sensors, inducing excessive production of IFN-I and other molecules known to play a key role in several autoimmune diseases, including SLE.
Previous studies found that mtDNA fragments are released from small holes (pores) located in the outer membrane of damaged mitochondria. How these pores form, however, was not known.
Using mouse embryonic cells, researchers at the National Heart Lung and Blood Institute and colleagues found that these pores form through a process called oligomerization in a protein known as voltage-dependent anion channel (VDAC). (Oligomerization is the process by which different subunits interact to form a more complex protein.)
VDAC sits on the outer membrane of mitochondria, and controls the flow of molecules. Specifically, the team discovered that the interaction between mtDNA fragments and a set of amino acids (the building blocks of proteins) in one of the terminals of VDAC1 — one of several VDAC proteins — was responsible for the creation of these pores.
Their work also showed that mitochondria with high levels of reactive oxygen species released mtDNA fragments into the cell’s cytosol through these small pores, leading to excessive production of IFN-I.
They found that this process could also be induced under milder stressful conditions, including microbial infections, suggesting that environmental factors may lead to excess levels of IFN-I.
“In a disease like lupus, there are many kinds of stressors that can trigger the disease or flares of the disease, such as ultraviolet light or excessive fatigue,” Mary K. Crow, MD, chair of the Department of Medicine at the Hospital for Special Surgery (HSS) and author of a perspective article about the study, said in a press release.
Researchers also found evidence of increased VDAC oligomerization in spleen cells isolated from a mouse model of SLE, and in white blood cells taken from patients with the disease.
When they treated SLE mice with VBIT-4, which blocks VDAC oligomerization, they found a lesser accumulation of mtDNA in the cytosol, lower activity of genes under the control of IFN-I, and a reduced production of autoantibodies.
“Thus, inhibiting VDAC oligomerization is a potential therapeutic approach for diseases associated with mtDNA release,” the investigators wrote.
But in her perspective article, Crow wrote: “Although inhibitors of the VDAC pore might be effective in reducing stimulatory mtDNA, the importance of the VDAC pore for transport of essential metabolites could complicate use of VDAC inhibitors as therapeutics for SLE or other disorders.”
Still, she noted that medications that block the activity of IFN-I, like AstraZeneca’s investigative treatment anifrolumab, seem to hold promise in helping those with SLE manage their disease.
Indeed, findings from the Phase 3 TULIP-2 (NCT02446899) trial showed that anifrolumab lowered disease activity, corticosteroid usage, and eased the severity of skin lesions in people with moderate-to-severe SLE.
“There is progress in developing therapies to inhibit interferon’s impact on the immune system and improve outcomes for patients with lupus,” Crow said.





