Lupus Researchers Uncover New Target to Prevent Vascular Complications in Certain Patients
Lupus patients with certain antibodies are more prone to getting blood clots, but researchers might have come up with a way of preventing such clots from forming in the first place.
In a new mouse study, researchers at the University of Michigan Medical School found that targeting the PSGL-1 molecule at the surface of neutrophils — the cells involved in clot formation — may possibly prevent these life-threatening events.
Their study, “Activated signature of antiphospholipid syndrome neutrophils reveals potential therapeutic target,” appeared in The Journal of Clinical Investigation.
The immune system protects against bacteria, viruses and disease-causing germs. But in autoimmune diseases, the immune system cannot distinguish healthy cells from foreign substance.
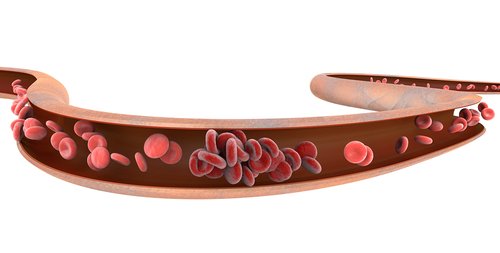
Nearly a third of all lupus patients have antiphospholipid antibodies, which put them at increased risk of developing clots in their blood vessels. As a consequence, they often die from clots, thrombotic events and other vascular complications. Yet in a condition called antiphospholipid syndrome (APS), these antibodies generally attach themselves to proteins on the membrane of blood cells.
One type of white blood cell that is crucial for thrombotic events are the neutrophils. When they encounter foreign substances, they must cross the blood vessel wall and enter infected tissues. To do so, neutrophils and endothelial cells — the cells that line blood vessels — interact through anchor-like proteins. This stops the neutrophil, allowing it to migrate.
Aiming to explain the increased likelihood of thrombosis in APS patients, researchers examined neutrophils from nine APS patients, and compared them to nine age-, sex- and ethnicity-matched healthy controls.
The team found 1,363 genes that were differentially expressed in APS and healthy neutrophils. This revealed a clear pro-inflammatory signature in APS cells. APS neutrophils also had higher levels of proteins involved in direct contact and adherence between neutrophils and endothelial cells.
After examining the function of each protein, researchers decided to further study the P-selectin glycoprotein ligand-1 (PSGL-1) protein in mice. This molecule, whose levels were 2.5 times higher in APS neutrophils, is a key initiator of contact between neutrophils and blood vessels. When scientists injected APS antibodies into control mice, it triggered a thrombotic effect — but that didn’t happen with mice deficient in PSGL-1. This indicates that antiphospholid antibodies need PSGL-1 to precipitate thrombosis events.
Most importantly, they showed that mice with neutrophils from APS patients had significantly smaller thrombosis size when treated with antibodies that attack this PSGL-1 protein.
“APS is an autoimmune disorder that is still primarily treated with anticoagulation, rather than immunomodulation,” authors wrote, but added that due to the inherent risk of anticoagulation treatment for APS, other treatment approaches should be pursued. “These data demonstrate the potential of PSGL-1 as a therapeutic target in APS. Our proof-of-principle data have demonstrated that antagonism of neutrophil adhesion can protect against thrombosis.”





