Lupus Might Be Treated with Electronic Manipulation of Nerves, Study Suggests
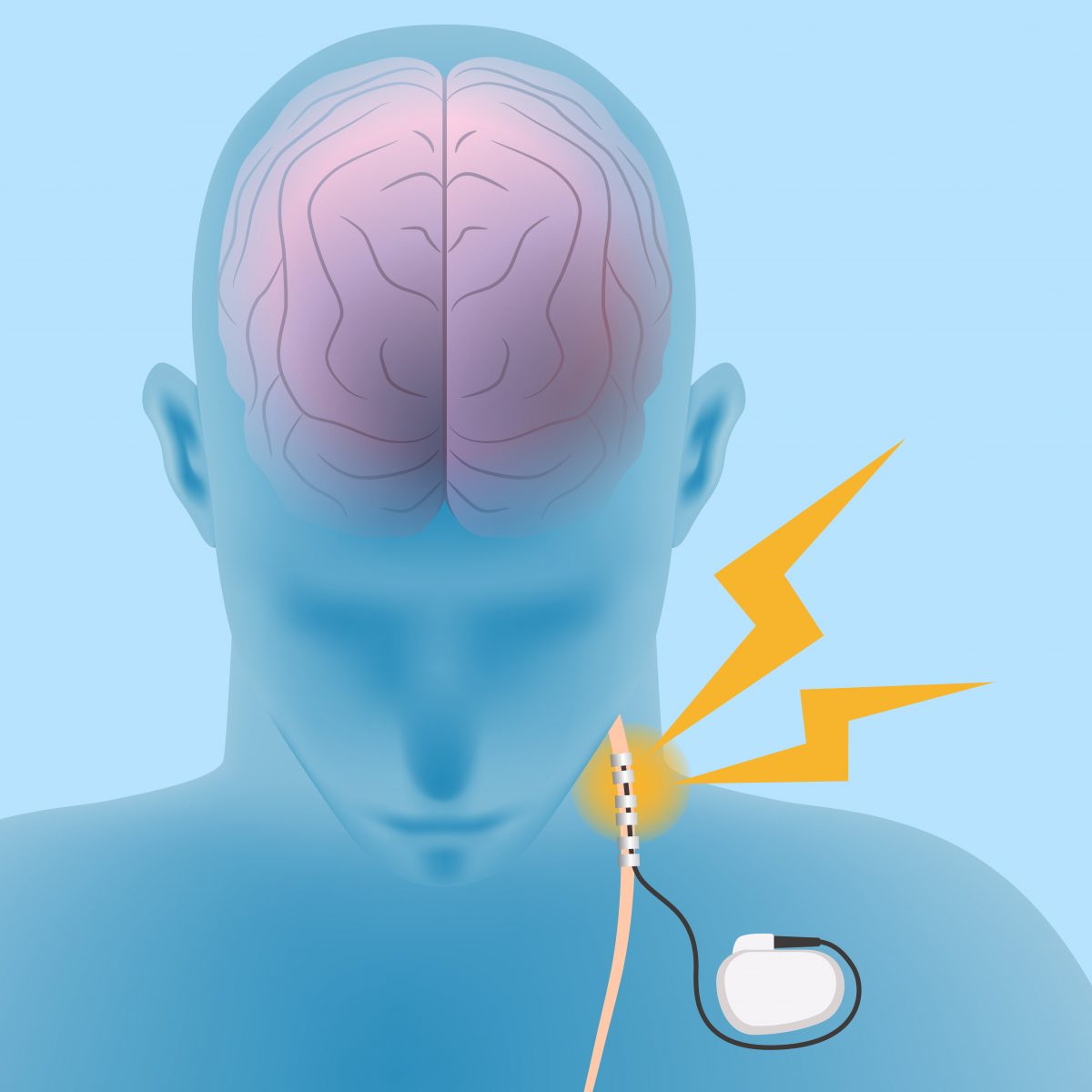
Researchers are learning how signals about disease-related inflammatory activity are sent from the body to the brain — insight that could lead to manipulating nerves to treat autoimmune conditions such as systemic lupus erythematosus.
A team at the Feinstein Institute for Medical Research in New York discovered that different immune mediators called cytokines trigger specific electric activity in the vagus nerve, the main route of communication between the immune system and the brain.
The study, “Cytokine-specific Neurograms in the Sensory Vagus Nerve,” was published in the journal Bioelectronic Medicine.
“We know from previous studies that the vagus nerve is a conduit for signals from many of our vital organs and that it has a role in reporting changes in inflammation to the brain,” Patricio Huerta, PhD, Feinstein Institute investigator and senior study author, said in a press release. “Our new finding clearly shows that the vagus nerve carries immune-related signals, which makes it a good target for bioelectronic treatment for autoimmune conditions such as rheumatoid arthritis, Crohn’s disease and lupus.”
Bioelectronic medicine is an emerging discipline that seeks to harness neural signals to treat disease. Scientists believe it could be applicable to non-nerve diseases as well as nerve diseases.
The vagus nerve sends information to the brain when, for instance, we get the flu. The signals can alter our behavior, inducing loss of appetite, for example. The brain can use the vagus nerve to send signals to the rest of the body, modulating the inflammatory response.
Researchers hope that harnessing the signals will lead to treatments for disease. But for this approach to work, they need to learn more about how nerve signals impact immune reactions in the body.
“In this study, we were looking to sharpen our understanding of what makes the vagus nerve sense the immune response,” Huerta said. “We devised an electrode setup to record down to the vagus fibers that are activated by the cytokines. We found that similar to how the brain perceives and interprets colors differently, each cytokine is perceived and interpreted by the vagus nerve differently.”
The team injected mice with one of two cytokines — TNF-alpha or IL-1beta. These factors are present in very low levels in healthy humans and animals, but are also involved in numerous diseases.
Using a new method to record signals from the vagus nerve, the researchers learned that each cytokine elicited signals at a specific frequency in the nerve.
The finding spurred the team to catalog the signals in the vagus nerve and the corresponding bodily reactions.
“Dr. Huerta and his team’s method of recording signals and identifying pathways within the nerve fiber opens up many new possibilities for our research teams to apply bioelectronic medicine to these nerves and treat many diseases and conditions,” concluded Kevin Tracey, MD, president and CEO of the Feinstein Institute.






