Lupus Researchers Find Mechanism in Stem Cell Transplants Known to Aid Bones
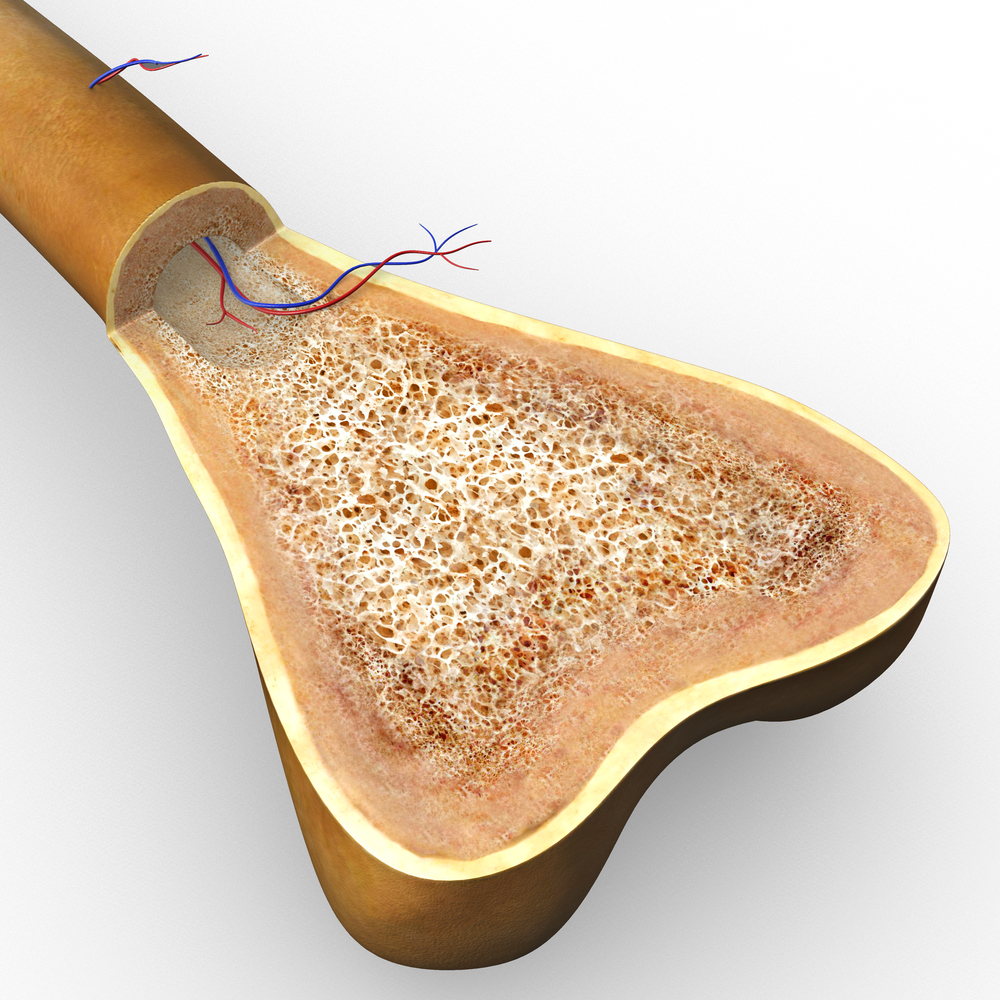
Transplanted mesenchymal stem cells that can differentiate into several types of cells are known to be beneficial in treating symptoms of lupus disease, though researchers were at a loss as to why. Now, scientists at the University of Pennsylvania, working with collaborators, have shed light on the mechanisms of bone protection provided by this therapy, showing that the transplanted cells are a source of a key protein called Fas, improving the function of bone marrow stem cells via a multi-step, epigenetic effect.
The paper resulting from their work, “MSC Transplantation Improves Osteopenia via Epigenetic Regulation of Notch Signaling in Lupus,” was published in Cell Metabolism and may potentially lead to new therapeutic strategies for lupus where stem cell transplantation has already shown some level of success.
In previous studies, the researchers observed that mesenchymal stem cell (MSC) transplantation was beneficial for the treatment of different autoimmune diseases, but the mechanisms underlying these therapeutic effects were elusive. To further investigate, they used a lupus mice model that had earlier shown amelioration — an ability to produce new bone — with one injection of the stem cells. MSC transplantation’s effects were reported as long as 12 weeks after the transfer.
“When we used stem cells for these diseases and put them into the circulation, we didn’t know exactly what they were doing but saw that they were very effective,” said Songtao Shi, chair and professor of the Department of Anatomy and Cell Biology in Penn’s School of Dental Medicine and a co-corresponding author on the paper, in a press release. “Now we’ve seen in a model of lupus that bone-forming mesenchymal stem cell function was rescued by a mechanism that was totally unexpected.”
The researchers also analyzed patterns of DNA methylation acting on the promoters of bone marrow mesenchymal stem cell genes, finding that lupus mice had a significantly different pattern than normal mice, but those differences were partly reversed by the stem cell therapy. Further studies revealed a malfunctioning Fas protein in the lupus mice that set into action a series of cell-level events that led their stem cells to differentiate poorly and them to have weaker bones. But healthy donated mesenchymal stem cells, infused into the lupus mice, secreted micro vesicles called exosomes that contained normal Fas that could be used by the diseased cells to restore their ability to self-renew and differentiate.
“The cells themselves don’t produce Fas, but they can use the components of the donor stem cells to rescue their function,” Shi said.
The results showed that mesenchymal stem cell transplant improves bone marrow function and alleviates the loss of bone protein and mineral content (osteopenia) in Fas-deficient mice models. The researchers now are planning to apply these lupus findings to other autoimmune diseases. “You can imagine if you can reuse Fas you might also be able to reuse other cell components to target other diseases,” added Shi.






