Study Explores How immune Cells Work Together in Inflammation
Despite intense research on autoimmune diseases like lupus, little is still known on how the immune system works to attack the patient’s tissues and organs. However, a recent study titled “Neutrophil trails guide influenza specific CD8+ T cells in the airways” and published early this month in the Science journal gives new insights on how immune cells work together towards their goal: destroy malignant cell and infectious agents.
Researchers from the University of Rochester School of Medicine and Dentistry looked at the response to flu infection in mice, in the hopes of understanding how immune cells behaved in the face of infection. They used a modern imaging technique called intravital multiphoton microscopy to analyze the behavior of the immune system in flu infected trachea (part of the respiratory system).
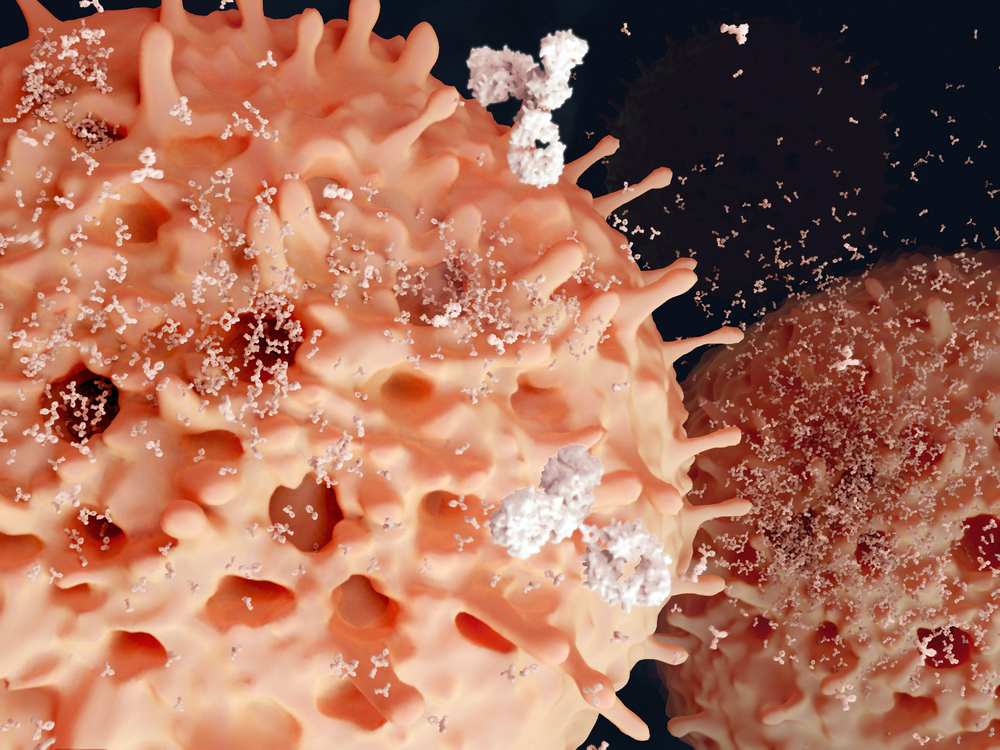
The team led by Professor Minsoo Kim found that specific cells called neutrophils are the first responders of the immune system. They belong to the so called innate immune system that normally recognizes generic pathogen signals or helps antibodies or immune cells destroy pathogenic cells. These neutrophil cells arrive at the site of infection within one hour and leave a chemical “trail” for specialized cells called cytotoxic T cells to follow.
Additionally, after removing these first responder cells (neutrophils) or their signals/”trails”, specialized T cells do not find the site of infection as easily as before and the ones that do are not as effective in fighting the infection.
Their results show that immune cells share information and team up to more effectively accomplish their goal of eradicating the infection and that the absence of a member of the team cripples the response to the insult.
Lupus is a is a chronic inflammatory disease that occurs when one’s immune system attacks healthy tissue. The specific causes of this behavior are still unknown but it is acknowledged that some drugs like Isoniazid, Hydralazine and Procainamide can induce SLE development. The pathology’s symptoms include joint pain, chest pain, fatigue, fever with no other cause, hair loss, among others.
These results are very encouraging. “In people with autoimmune disorders like multiple sclerosis and lupus, the immune system mistakenly attacks and destroys healthy body tissue. If scientists understood how to disrupt or stop immune cells’ movement to healthy tissue, they may be able to improve the quality of life of people living with these devastating diseases,” the authors explained. The study therefore shows the importance of scientific research, especially regarding clinical trials and clinical studies in humans in these lifelong and severe diseases for a hope of a better therapeutic approach.





