Microbial Biofilms Connected To Autoimmune Diseases
The role of biofilms, until recently, had been studied mostly in reference to bacterial deposition, protection and antibiotic resistance acquired by groups of bacteria due to formation of these structures. However, recent studies by a group of researchers at Temple University School of Medicine (TUSM) have shown that bacterial communities forming biofilms play a role in the development of the autoimmune disease systemic lupus erythematosus (SLE) – something that might provide important insights on autoimmune diseases as a whole.
The research team led by TUSM researchers, Çagla Tükel, PhD, an Assistant Professor of Microbiology and Immunology at TUSM, and Stefania Gallucci, MD, Associate Chair, Microbiology and Immunology, as well as an Associate Professor in Microbiology and Immunology at TUSM (both members of the Temple Autoimmune Center) studied the effects of biofilm formation by common gut bacteria, Eschereichia coli (E.coli) and Salmonella typhimurium, a common bacterium associated with food borne infections and their possible effects on SLE and its flare-ups.
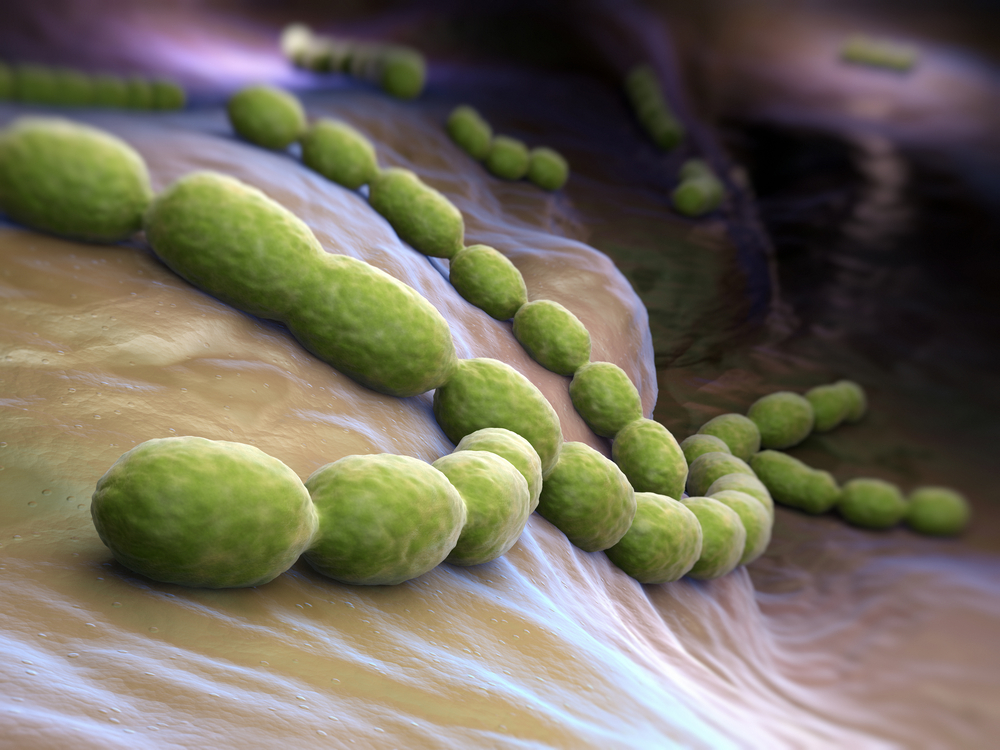
Biofilms, proteinaceous layers of bacterial films, are formed within the alimentary canal (by gut bacteria), on urinary catheters (by nosocomial bacteria) or as dental plaques (due to oral bacteria). Some of these biofilms have DNA excreted by E.coli and Salmonella, along with proteins known as amyloids (biofilms formed as a result of amyloids referred to as curli). Amyloids along with this excretory DNA form strong bonds which are difficult to break. This DNA-curli complex forms the crux of autoimmune attacks on the SLE host.
Studies in SLE prone mice (who were predisposed to the condition due to genetic factors) have shown that immune cells (dendritic cells) when in contact with these DNA-curli complexes released massive amounts of pro-inflammatory cytokines, which induce autoimmune responses and produce auto-antibodies, much in similarity to that against pathogenic lipopolysachharide complexes (LPS). Different classes of mice, with and without genetic predisposition to SLE also developed the condition with varying severities upon injection with these DNA-curli complexes.
Knowing that bacterial infections lead to as much as 55% flare-ups in cases of lupus, it was not a difficult task to conclude that bacterial biofilms played a crucial role in development of autoimmune conditions in host systems.
Further research on this topic could shed considerable light on other diseases like Alzheimer’s disease, type-2 diabetes and Parkinson’s disease which also features amyloids.
“The next step is to explore the mechanism of how these composites are stimulating autoimmunity,” Dr. Tükel said. “The beneficial bacteria found in our guts can cause problems when they cross the intestinal barrier and reach to places they shouldn’t be. Thus, besides infectious bacteria, a leaky gut could cause many problems. We are now starting to understand how the bacteria in our gut may trigger complex human diseases including lupus. So it’s critical for us to understand the biology of the bacterial communities and their interactions with the immune system.”
“Understanding how biofilms trigger autoimmunity may ultimately lead to changes in patient treatment” Dr. Gallucci said, “So understanding how the biofilms affect flares could lead to a different treatment approach. Now, they give immune suppressive drugs. Maybe you want to do something else, like treat the underlying infection.”





