Platelets Play Role in Exacerbated Immune Response in Lupus, Mouse Study Suggests
In addition to their role in coagulation and healing, platelets seem to be involved in the response to foreign invaders like bacteria and viruses, contributing to an exacerbated immune response, a new study shows.
The research, published in Proceedings of the National Academy of Sciences (PNAS), suggests that platelets play a much wider role in the immune system than previously thought, opening the door to new ways of treating autoimmune diseases like lupus.
Our immune system is a learning and memory platform, allowing it to fulfill its functions of defense against foreign invaders. After an initial attack by a virus or bacteria, for example, the immune system develops antibodies that are capable of recognizing specific molecules (antigens) of the invaders. In a second encounter with the same bacteria or virus, these antibodies rapidly attach to the antigens forming an antibody-antigen complex that then triggers an immune response.
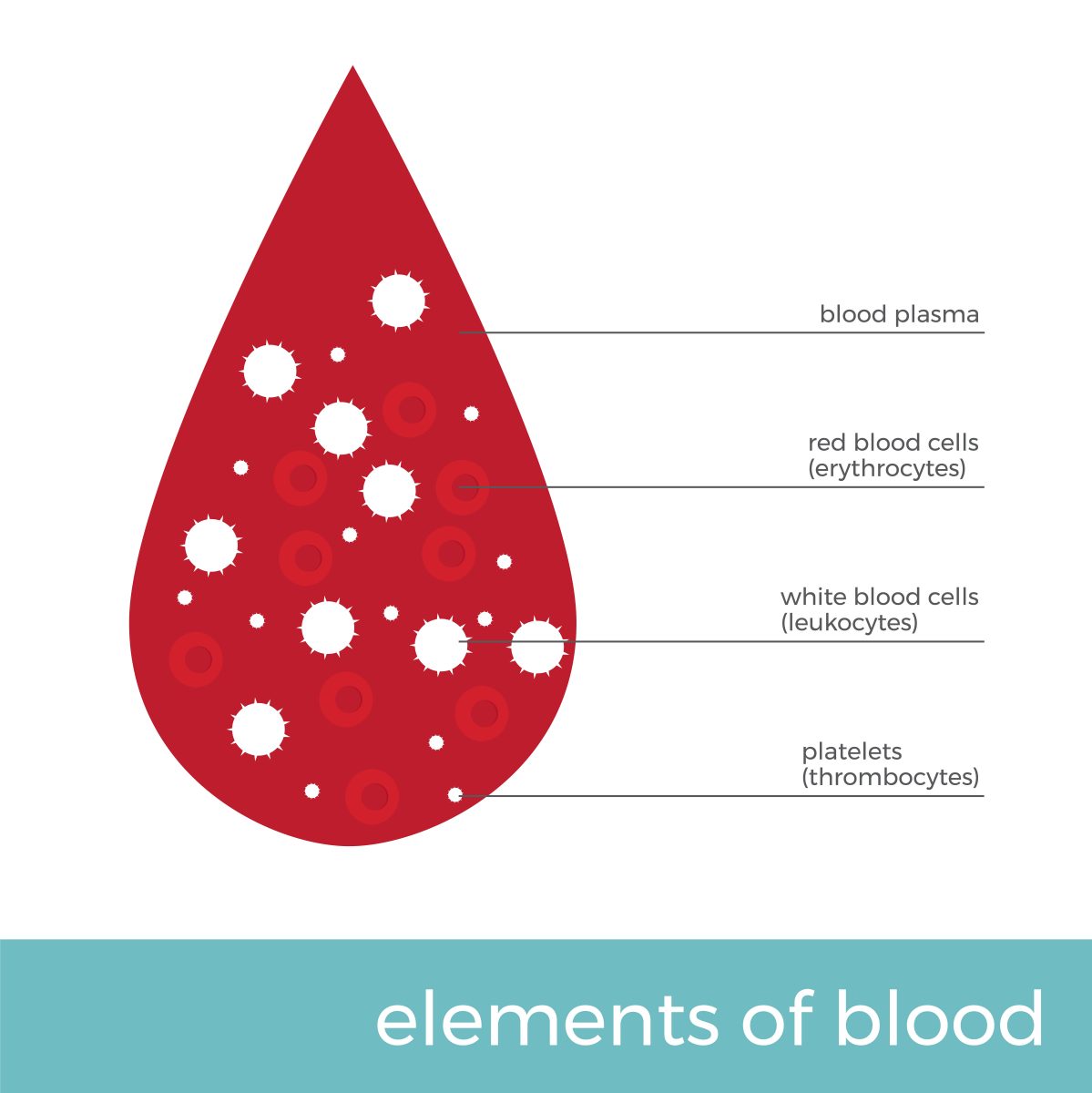
Platelets — the small disc-shaped cells found in blood circulation — have receptors that are capable of recognizing these antibody-antigen complexes, which led researchers to hypothesize that platelets could play a role in inflammation.
In the study, “Platelets release pathogenic serotonin and return to circulation after immune complex-mediated sequestration,” researchers tested their hypothesis and used different types of foreign invaders — a virus, a bacterial toxin, and an allergen — to create antigen-antibody complexes in the blood of mice.
All three different complexes led to classic symptoms of septic or anaphylactic shock, both of which characterized by an abnormal, exacerbated immune response, including body temperature drop, tremors, and impaired cardiac function. These reactions led to vasodilation and eventually loss of consciousness.
But in mice without platelets, those effects were absent.
“We repeated the tests on mice with almost all platelets removed and on mice with no antigen-antibody complex receptors on their platelets. These mice had no physiological response, which clearly demonstrates the key role of platelets in the process. Platelets, and not white blood cells, are first on the scene during an immune response,” explained study lead author Éric Boilard, PhD, and a professor at the Université Laval Faculty of Medicine, Canada in a press release.
Subsequent experiments found that mice entered in shock because platelets released serotonin (a neurotransmitter) into the blood within 10 minutes after administration of the antigen-antibody complexes.
“It’s the same molecule as the neurotransmitter in the brain, but the molecule in the platelets is produced by cells in the intestine. Platelets store serotonin — they contain 90% of the body’s entire serotonin supply — and release it in certain situations,” Boilard explained.
These findings carry significant clinical implications. For example, platelet transfusion in patients who already are in septic or anaphylactic shock may worsen their status by increasing the levels of serotonin in the blood.
“Transfusion remains important, especially since those patients often show low platelet levels, but in order to prevent the problem the antigen-antibody complex receptors on the platelets should be blocked before transfusion,” Boilard said.
Patients with rheumatic diseases like lupus also carry antigen-antibody complexes that activate platelets, suggesting that interfering with platelets’ capacity to respond to these complexes might be a promising avenue for further research.
“We believe that by blocking the receptor [for the antibody-antigen complexes], we should be able to improve a patient’s condition without affecting everything else that platelets do,” Boilard concluded.






