Lupus Review Cites Prevalence of Central Nervous System Involvement
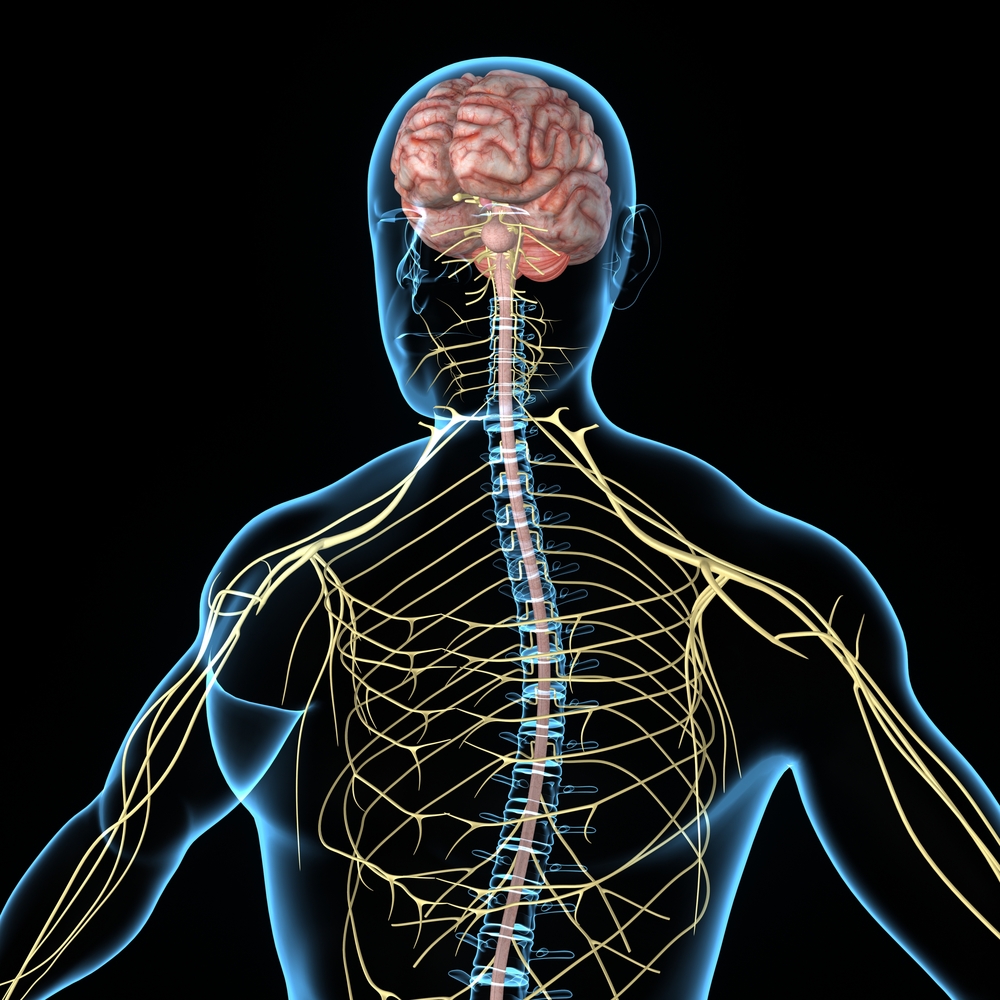
A recent systematic review, published in the International Journal of Chronic Diseases, revealed the prevalence of the central nervous system (CNS) involvement — rather than the peripheral nervous system (PNS) — in connective tissue disorders like systemic lupus erythematosus. But more research is needed to understand whether these CNS or PNS complications are direct or secondary effects in these diseases.
The review study is titled “A Systematic Review of Peripheral and Central Nervous System Involvement of Rheumatoid Arthritis, Systemic Lupus Erythematosus, Primary Sjögren’s Syndrome, and Associated Immunological Profiles.”
Connective tissue disorders are chronic inflammatory autoimmune disorders caused by an antibody or T-cell response against a self-antigen antibody disturbing the skin, the joints, and the muscles. These include diseases such as systemic lupus erythematosus (SLE), rheumatoid arthritis (RΑ), primary Sjögren’s syndrome (pSS), and systemic sclerosis (SSc). Immune mediated alterations in the vasculature of the vessels walls may be linked with central nervous system (CNS) and peripheral nervous system (PNS) symptoms. However, the most common CNS and PNS complications of these diseases, with an emphasis on their associated immunological features, remain unclear.
In the review, Anastasia Bougea from the Department of Neurology, University of Athens Medical School, Eginition Hospital, in Greece, and colleagues conducted a systematic review of databases (Medline, Scopus, and Cochrane Library) from 1989 to 2014, searching for relevant studies into specific connective tissue disorders, including SLE, that considered peripheral and central nervous complications and immunological profiles.
The review revealed that the majority of reported studies found CNS manifestations in 13% to 92% of SLE events compared to 8%–56% for the PNS, a finding consistent with previous studies in which CNS manifestations in SLE ranged from 33% to 75%. Overall, CNS complications (9%–92%) were found to be much more frequent than PNS complications (8%–66%) across the 22 studies included in the review, comprising a total of 2,338 connective tissue disease patients.
“It is still a matter of debate whether the CNS and PNS manifestations of RA, SLE, and pSS are direct effect of these diseases or secondary, such as side effects of corticosteroids and other immunosuppressive therapies or multiple systemic organ dysfunction (i.e., drug or SLE-mediated multiorgan induced psychosis). Τo date, no laboratory test, that is, autoantibodies, has been shown as pathognomonic neither for CNS nor for PNS involvement in these connective tissue disorders. Prospective multicenter studies are warrant for further confirmations,” the authors concluded.






